Gestational Diabetes
Overview
Gestational diabetes mellitus (GDM) is a type of diabetes that develops during pregnancy, typically in the second or third trimester. It occurs when the body cannot produce enough insulin to meet the increased needs during pregnancy, leading to high blood sugar levels. GDM can affect both the mother’s and baby’s health if not properly managed.
Causes
- Hormonal Changes: Pregnancy hormones can interfere with the action of insulin, leading to insulin resistance.
- Increased Insulin Demand: The growing baby and placenta produce hormones that increase the body’s need for insulin, sometimes beyond what the pancreas can produce.
- Risk Factors:
- Obesity
- Previous history of gestational diabetes
- Family history of diabetes
- Age (older than 25)
- Ethnicity (higher risk in African American, Hispanic, Native American, and Asian women)
Symptoms
Gestational diabetes often does not cause noticeable symptoms. When symptoms do occur, they may include:
- Increased thirst
- Frequent urination
- Fatigue
- Blurred vision
Diagnosis
GDM is typically diagnosed through screening tests during pregnancy:
- Glucose Challenge Test (GCT): A preliminary screening test where the patient drinks a glucose solution, and blood sugar levels are measured after one hour. If the levels are high, further testing is required.
- Oral Glucose Tolerance Test (OGTT): A more definitive test involving fasting overnight, drinking a glucose solution, and having blood sugar levels measured at intervals over three hours.
Treatment
Effective management of gestational diabetes is crucial to ensure a healthy pregnancy and delivery. Treatment options include:
Dietary Changes:
- Eat balanced meals with appropriate portions of carbohydrates, proteins, and fats.
- Monitor carbohydrate intake to prevent spikes in blood sugar.
- Include fiber-rich foods like vegetables, fruits, and whole grains.
- Avoid sugary foods and beverages.
Physical Activity:
- Regular moderate exercise can help control blood sugar levels.
- Activities like walking, swimming, and prenatal yoga are often recommended.
Blood Sugar Monitoring:
- Frequent monitoring of blood sugar levels is essential to ensure they remain within the target range.
- Patients may need to check their blood sugar multiple times a day using a glucose meter.
Medication:
- If blood sugar levels cannot be controlled through diet and exercise, insulin therapy may be required.
- In some cases, oral diabetes medications may be prescribed.
Regular Prenatal Care:
- Regular check-ups with the healthcare provider to monitor the health of both mother and baby.
- Ultrasounds and other tests may be performed to monitor the baby’s growth and development.
Risks and Complications
Uncontrolled gestational diabetes can lead to complications for both the mother and the baby:
For the Baby:
- Macrosomia: Larger than average baby, which can lead to delivery complications.
- Hypoglycemia: Low blood sugar after birth.
- Respiratory Distress Syndrome: Difficulty breathing due to underdeveloped lungs.
- Jaundice: Yellowing of the skin and eyes.
- Increased risk of obesity and type 2 diabetes later in life.
For the Mother:
- Pre-eclampsia: High blood pressure and signs of damage to another organ system.
- Increased risk of cesarean delivery.
- Higher risk of developing type 2 diabetes in the future.
Postpartum Care
Blood Sugar Monitoring:
- Blood sugar levels are typically monitored closely after delivery to ensure they return to normal.
- Women who have had GDM should have a glucose tolerance test 6-12 weeks postpartum to check for persistent diabetes.
Long-Term Health:
- Maintaining a healthy weight, balanced diet, and regular physical activity can help reduce the risk of developing type 2 diabetes later in life.
- Regular screening for diabetes is recommended for women who had gestational diabetes.
Conclusion
Gestational diabetes is a manageable condition with the right approach, involving dietary changes, regular physical activity, blood sugar monitoring, and medical care. Proper management ensures a healthy pregnancy and reduces the risk of complications for both the mother and the baby. Regular follow-up and postpartum care are crucial to prevent long-term health issues.
Hypertensive Disorders in Pregnancy
Overview
Hypertensive disorders during pregnancy are conditions characterized by high blood pressure that can significantly impact the health of both the mother and the baby. These disorders are classified into several categories, including chronic hypertension, gestational hypertension, preeclampsia, and eclampsia.
Types of Hypertensive Disorders
Chronic Hypertension:
- High blood pressure that is present before pregnancy or diagnosed before 20 weeks of gestation.
- It persists beyond 12 weeks postpartum.
Gestational Hypertension:
- High blood pressure that develops after 20 weeks of pregnancy without protein in the urine or other signs of preeclampsia.
- Blood pressure usually returns to normal postpartum.
Preeclampsia:
- A severe condition that occurs after 20 weeks of pregnancy, characterized by high blood pressure and signs of damage to other organ systems, often the kidneys (indicated by protein in the urine).
- Can develop into eclampsia if left untreated.
Eclampsia:
- A severe form of preeclampsia that involves seizures.
- It is a medical emergency that requires immediate treatment to prevent maternal and fetal mortality.
Chronic Hypertension with Superimposed Preeclampsia:
- Women with chronic hypertension who develop worsening high blood pressure and protein in the urine or other symptoms of preeclampsia.
Causes and Risk Factors
- Genetics: Family history of hypertension or preeclampsia.
- Obesity: Higher body mass index (BMI) increases risk.
- First Pregnancy: Higher incidence in first-time mothers.
- Age: Women over 35 have a higher risk.
- Multiple Gestations: Carrying twins or more.
- Underlying Conditions: Pre-existing conditions such as diabetes, kidney disease, or autoimmune disorders.
Symptoms
Chronic Hypertension: May be asymptomatic or cause headaches and vision changes.
Gestational Hypertension: Usually asymptomatic; detected through routine blood pressure monitoring.
Preeclampsia:
- Severe headaches
- Visual disturbances (blurring, flashing lights)
- Upper abdominal pain, usually under the ribs on the right side
- Nausea or vomiting
- Swelling, particularly in the face and hands
- Sudden weight gain
- Shortness of breath (due to fluid in the lungs)
Eclampsia: Seizures, loss of consciousness, severe agitation, or altered mental state.
Diagnosis
- Blood Pressure Measurement: Consistently high readings (≥140/90 mmHg).
- Urine Tests: Checking for proteinuria.
- Blood Tests: To assess liver function, kidney function, and platelet count.
- Fetal Monitoring: Ultrasounds and non-stress tests to monitor fetal well-being.
- Other Tests: Assessing for symptoms and signs of organ damage.
Treatment
Chronic Hypertension:
- Medications: Safe antihypertensive medications for pregnancy, such as methyldopa, labetalol, or nifedipine.
- Monitoring: Frequent prenatal visits to monitor blood pressure and fetal growth.
Gestational Hypertension:
- Monitoring: Regular blood pressure checks and fetal monitoring.
- Medications: Antihypertensives if blood pressure is significantly elevated.
Preeclampsia:
- Hospitalization: Severe cases may require hospital admission for close monitoring.
- Medications: Antihypertensives and magnesium sulfate to prevent seizures.
- Delivery: The only definitive treatment is delivery, typically recommended if the condition is severe or the pregnancy is at term.
Eclampsia:
- Emergency Care: Immediate medical intervention to control seizures and stabilize the mother.
- Delivery: Urgent delivery is usually necessary to protect both mother and baby.
Risks and Complications
For the Mother:
- Placental abruption
- HELLP syndrome (Hemolysis, Elevated Liver enzymes, Low Platelet count)
- Stroke
- Organ damage (kidneys, liver)
- Increased risk of cardiovascular disease later in life
For the Baby:
- Preterm birth
- Intrauterine growth restriction (IUGR)
- Low birth weight
- Stillbirth
- Respiratory distress syndrome (if born prematurely)
Postpartum Care
- Monitoring: Blood pressure monitoring postpartum, as hypertensive disorders can persist or develop after delivery.
- Medications: Continued antihypertensive treatment if needed.
- Follow-Up: Regular follow-up visits to monitor blood pressure and manage any long-term effects.
Conclusion
Hypertensive disorders during pregnancy require careful monitoring and management to ensure the health and safety of both mother and baby. Early detection through routine prenatal care, appropriate treatment, and timely delivery can help mitigate risks and improve outcomes.
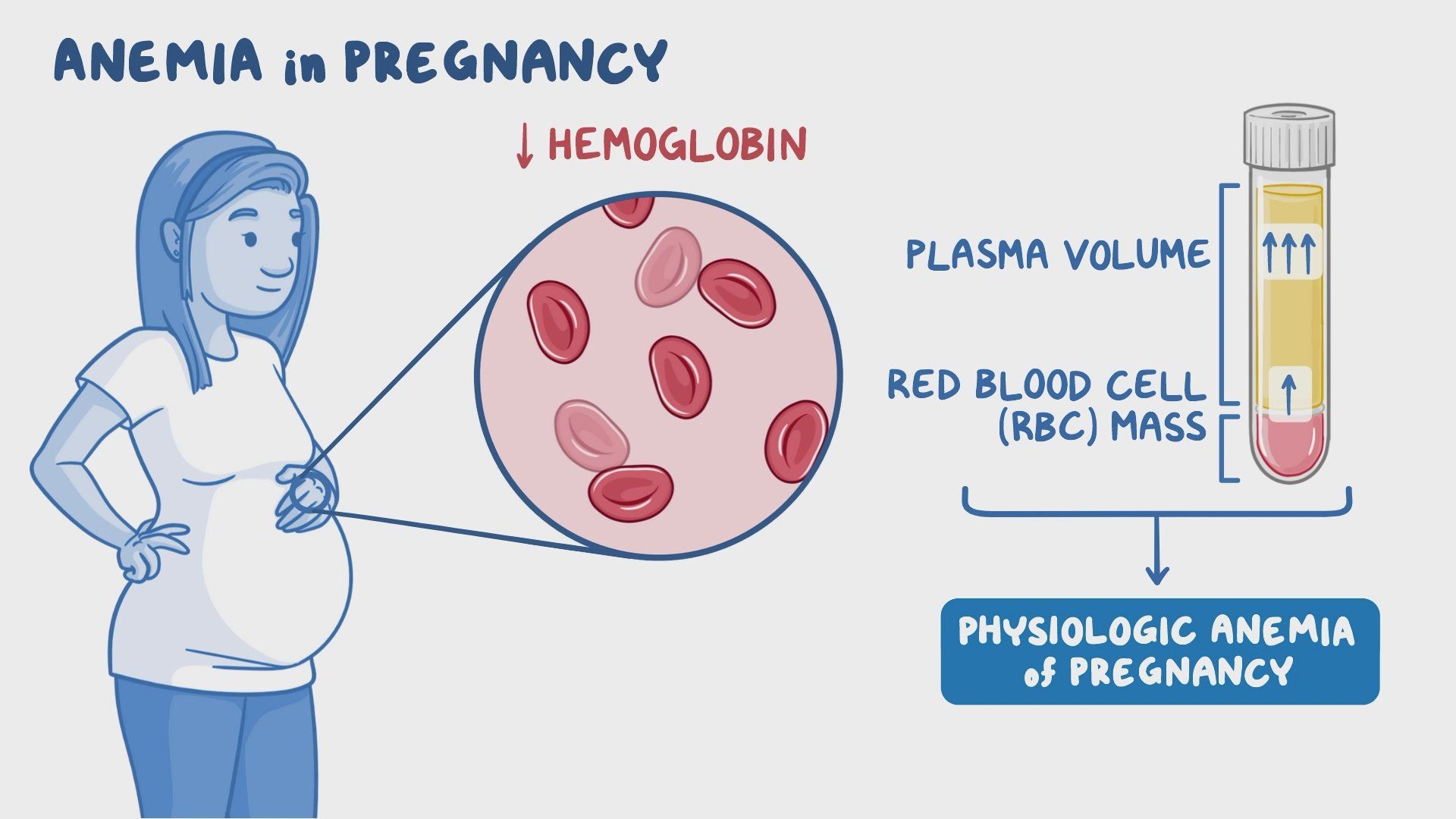
Anemia in Pregnancy
Overview
Anemia during pregnancy is a condition in which a woman’s blood has a lower than normal number of red blood cells or hemoglobin, leading to reduced oxygen transport to the body’s tissues and organs. It is common in pregnancy due to increased blood volume, and if severe, it can pose risks to both the mother and the baby.
Types of Anemia in Pregnancy
- Iron-Deficiency Anemia: The most common type, caused by a lack of iron, which is essential for hemoglobin production.
- Folate-Deficiency Anemia: Caused by a lack of folate (vitamin B9), necessary for red blood cell formation.
- Vitamin B12 Deficiency Anemia: Less common, but occurs when there is insufficient vitamin B12 for red blood cell production.
Causes
- Increased Blood Volume: During pregnancy, blood volume increases by about 50%, diluting the red blood cells.
- Inadequate Nutrient Intake: Poor dietary intake of iron, folate, or vitamin B12.
- Frequent Pregnancies: Closely spaced pregnancies can deplete iron stores.
- Loss of Blood: Bleeding due to conditions like placenta previa, or hemorrhoids.
- Chronic Conditions: Conditions like kidney disease can affect red blood cell production.
Symptoms
- Fatigue and weakness
- Pale or sallow skin
- Shortness of breath
- Dizziness or lightheadedness
- Rapid or irregular heartbeat
- Chest pain
- Cold hands and feet
- Headaches
Diagnosis
- Complete Blood Count (CBC): Measures levels of hemoglobin, hematocrit, and red blood cells.
- Iron Studies: Assess serum ferritin, serum iron, total iron-binding capacity (TIBC), and transferrin saturation.
- Vitamin Levels: Measure serum levels of folate and vitamin B12.
- Peripheral Blood Smear: Microscopic examination of red blood cells to identify abnormalities.
Treatment
Iron-Deficiency Anemia:
- Dietary Changes: Increase intake of iron-rich foods such as red meat, poultry, fish, lentils, beans, spinach, and iron-fortified cereals.
- Iron Supplements: Oral iron supplements (ferrous sulfate, ferrous gluconate) are commonly prescribed. Intravenous iron may be necessary for severe cases or if oral iron is not tolerated.
- Vitamin C: Enhances iron absorption when taken with iron-rich foods or supplements.
Folate-Deficiency Anemia:
- Dietary Changes: Increase intake of folate-rich foods such as leafy green vegetables, citrus fruits, beans, and fortified cereals.
- Folic Acid Supplements: Recommended daily folic acid supplement of 400-800 micrograms for pregnant women.
Vitamin B12 Deficiency Anemia:
- Dietary Changes: Increase intake of vitamin B12-rich foods such as meat, dairy products, eggs, and fortified cereals.
- Vitamin B12 Supplements: Oral or injectable vitamin B12 supplements if dietary intake is insufficient.
Risks and Complications
For the Mother:
- Severe fatigue and weakness
- Increased risk of infections
- Preterm labor and delivery
- Postpartum depression
- Poor wound healing
For the Baby:
- Low birth weight
- Preterm birth
- Developmental delays
- Increased risk of infant mortality
Prevention
- Balanced Diet: Ensure a well-rounded diet rich in iron, folate, and vitamin B12.
- Prenatal Vitamins: Regular use of prenatal vitamins containing iron and folic acid.
- Routine Screening: Regular screening for anemia during prenatal visits to detect and treat early.
- Spacing Pregnancies: Allow sufficient time between pregnancies to replenish nutrient stores.
Postpartum Care
- Continued Supplementation: Continued use of iron and folic acid supplements postpartum, especially if breastfeeding.
- Dietary Counseling: Guidance on maintaining a nutrient-rich diet to prevent recurrence.
- Follow-Up Testing: Regular blood tests to monitor hemoglobin levels and overall health.
Conclusion
Anemia in pregnancy is a manageable condition with proper diagnosis, treatment, and prevention strategies. Early detection through routine prenatal care, appropriate dietary adjustments, and supplementation can help ensure a healthy pregnancy and reduce risks for both mother and baby
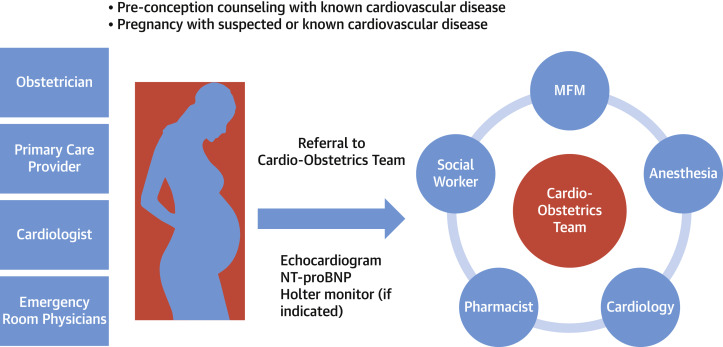
Cardiac Disorders in Pregnancy
Overview
Cardiac disorders during pregnancy are medical conditions that affect the heart and can complicate pregnancy, posing risks to both the mother and the fetus. These conditions may be pre-existing or develop during pregnancy. Managing cardiac disorders in pregnant women requires a multidisciplinary approach to ensure optimal outcomes for both mother and baby.
Common Cardiac Disorders in Pregnancy
Congenital Heart Disease (CHD): Heart defects present from birth. Common examples include atrial septal defect, ventricular septal defect, and tetralogy of Fallot.
Acquired Heart Disease: Conditions developed after birth, such as:
- Rheumatic Heart Disease: Resulting from rheumatic fever, affecting the heart valves.
- Cardiomyopathy: Disease of the heart muscle, including peripartum cardiomyopathy, which occurs in the last month of pregnancy or within five months postpartum.
- Coronary Artery Disease: Blockage or narrowing of coronary arteries, leading to reduced blood flow to the heart.
Hypertensive Disorders: Includes chronic hypertension, gestational hypertension, and preeclampsia, which can strain the heart.
Arrhythmias: Abnormal heart rhythms, such as atrial fibrillation, which may be more frequent during pregnancy.
Causes and Risk Factors
- Pre-existing Heart Conditions: Women with pre-existing cardiac disorders are at higher risk.
- Advanced Maternal Age: Older age increases the risk of cardiac complications.
- Obesity: Excess weight can strain the heart and lead to complications.
- Multiple Gestations: Carrying twins or more increases cardiovascular demand.
- Diabetes and Hypertension: These conditions can exacerbate cardiac issues.
Symptoms
- Shortness of breath
- Chest pain
- Palpitations
- Fatigue
- Swelling of the legs, ankles, or feet
- Dizziness or fainting
Diagnosis
- Physical Examination: Listening for abnormal heart sounds and checking for signs of heart failure.
- Electrocardiogram (ECG): Measures the electrical activity of the heart.
- Echocardiogram: Uses ultrasound to create images of the heart and assess its function.
- Blood Tests: To check for markers of heart stress or damage.
- Cardiac MRI or CT Scan: Detailed imaging to evaluate heart structures and function, used selectively to minimize radiation exposure.
Treatment
Medications:
- Antihypertensives: To manage high blood pressure (e.g., labetalol, nifedipine).
- Diuretics: To reduce fluid buildup in heart failure (used cautiously).
- Antiarrhythmics: To control abnormal heart rhythms.
- Anticoagulants: To prevent blood clots in certain conditions (e.g., heparin).
Lifestyle Modifications:
- Dietary Changes: Low-sodium, heart-healthy diet.
- Physical Activity: Gentle, regular exercise as advised by a healthcare provider.
- Weight Management: Maintaining a healthy weight through balanced nutrition.
Monitoring and Follow-Up:
- Regular prenatal visits with a multidisciplinary team including obstetricians, cardiologists, and anesthesiologists.
- Frequent monitoring of heart function and fetal well-being.
Delivery Planning:
- Mode of Delivery: Vaginal delivery is often preferred, but cesarean section may be necessary depending on the cardiac condition.
- Anesthesia Management: Tailored to minimize cardiovascular stress during delivery.
- Postpartum Care: Close monitoring for heart failure and other complications in the immediate postpartum period.
Risks and Complications
For the Mother:
- Heart failure
- Arrhythmias
- Thromboembolism (blood clots)
- Worsening of existing cardiac conditions
For the Baby:
- Preterm birth
- Low birth weight
- Growth restriction
- Increased risk of congenital heart disease (if the mother has a genetic heart condition)
Postpartum Care
- Continued Monitoring: Close follow-up to manage any lingering or new cardiac issues.
- Medications: Adjustment of medications as needed, considering breastfeeding safety.
- Education and Support: Counseling on symptoms to watch for and lifestyle modifications to maintain heart health.
Conclusion
Cardiac disorders in pregnancy require careful management to ensure the health and safety of both the mother and the baby. Early diagnosis, appropriate treatment, and close monitoring are crucial for preventing complications and promoting a healthy pregnancy outcome. A collaborative approach involving cardiologists, obstetricians, and other healthcare providers is essential for optimal care.
Intrahepatic Cholestasis of Pregnancy (ICP)
Overview
Intrahepatic Cholestasis of Pregnancy (ICP) is a liver disorder that occurs during pregnancy. It is characterized by impaired bile flow, leading to the accumulation of bile acids in the liver and bloodstream. ICP typically presents in the third trimester and resolves after delivery.
Causes and Risk Factors
- Genetic Predisposition: Family history of ICP increases risk.
- Hormonal Changes: Elevated levels of pregnancy hormones, particularly estrogen and progesterone, can impair bile flow.
- Environmental Factors: Certain environmental factors, such as diet, can influence the risk.
- Pre-existing Liver Conditions: Women with pre-existing liver conditions may be more susceptible to developing ICP.
Symptoms
- Intense Itching (Pruritus): Most commonly on the palms of the hands and soles of the feet, but it can occur anywhere on the body. Itching is usually worse at night.
- Dark Urine: Due to increased bile pigments in the urine.
- Pale Stools: Resulting from decreased bile excretion.
- Jaundice: Yellowing of the skin and eyes, although this is less common.
- Fatigue and Malaise: General feeling of discomfort and tiredness.
Diagnosis
- Liver Function Tests (LFTs): Elevated levels of liver enzymes (ALT, AST).
- Serum Bile Acid Test: Elevated bile acid levels in the blood are a key diagnostic marker.
- Ultrasound: To rule out other liver or gallbladder conditions.
- History and Physical Examination: Evaluation of symptoms and family history.
Treatment
Medications:
- Ursodeoxycholic Acid (UDCA): The primary treatment to improve liver function, reduce bile acids, and alleviate itching.
- Antihistamines: To help manage itching, though they are less effective than UDCA.
- Cholestyramine: Occasionally used to reduce bile acids, but its use is limited due to potential interference with the absorption of other medications and vitamins.
Monitoring and Follow-Up:
- Frequent Liver Function Tests: To monitor liver enzymes and bile acid levels.
- Fetal Monitoring: Regular non-stress tests and biophysical profiles to monitor fetal well-being.
Delivery Planning:
- Early Delivery: Often recommended at around 37-38 weeks to reduce the risk of fetal complications.
- Cesarean Section: Considered if there are other obstetric indications.
Risks and Complications
For the Mother:
- Increased risk of postpartum hemorrhage due to reduced vitamin K absorption and associated clotting issues.
- Recurrence in future pregnancies.
For the Baby:
- Preterm birth
- Fetal distress
- Meconium-stained amniotic fluid
- Stillbirth (rare but serious risk)
Postpartum Care
- Resolution of Symptoms: Symptoms usually resolve within days to weeks after delivery.
- Follow-Up Tests: Liver function and bile acid levels should be rechecked postpartum to ensure normalization.
- Future Pregnancies: Counseling on the high likelihood of recurrence in subsequent pregnancies.
Conclusion
Intrahepatic Cholestasis of Pregnancy is a manageable condition with timely diagnosis and appropriate treatment. Close monitoring and management can help mitigate risks and ensure the health and safety of both the mother and the baby. Early delivery is often considered to reduce the risk of fetal complications. Women with a history of ICP should be closely monitored in future pregnancies for early detection and management of the condition.
Rh-Negative Pregnancy
Overview
Rh-negative pregnancy refers to a situation where a pregnant woman has Rh-negative blood type and her fetus has Rh-positive blood type, inherited from the father. This can lead to Rh incompatibility, which might cause complications such as hemolytic disease of the newborn (HDN).
The Rh Factor
- Rh Factor: A protein found on the surface of red blood cells. People who have it are Rh-positive, and those who don’t are Rh-negative.
- Rh Incompatibility: Occurs when an Rh-negative mother is pregnant with an Rh-positive baby. The mother’s immune system may produce antibodies against the baby’s Rh-positive blood cells.
Causes and Risk Factors
- Genetics: The Rh factor is inherited. Rh-negative status is less common than Rh-positive.
- Previous Pregnancies: The risk of Rh incompatibility increases with each subsequent Rh-positive pregnancy if not properly managed.
- Blood Transfusions: Receiving Rh-positive blood can sensitize an Rh-negative person.
Mechanism of Rh Incompatibility
- Sensitization: If an Rh-negative woman is exposed to Rh-positive blood, her immune system may produce antibodies against Rh-positive cells.
- Subsequent Pregnancies: In future Rh-positive pregnancies, these antibodies can cross the placenta and attack the fetus’s red blood cells, causing hemolytic disease of the newborn.
Symptoms of Hemolytic Disease of the Newborn (HDN)
- Mild Cases: May have no symptoms or only mild anemia.
- Severe Cases: Jaundice, anemia, enlarged liver and spleen, heart failure, and severe swelling (hydrops fetalis).
Diagnosis
- Blood Type Testing: Determines the Rh status of the mother and, if possible, the father.
- Antibody Screening: Tests for the presence of Rh antibodies in the mother’s blood.
- Fetal Monitoring:
- Ultrasound: To check for signs of fetal anemia or hydrops fetalis.
- Amniocentesis: Measures bilirubin levels in amniotic fluid.
- Middle Cerebral Artery Doppler: Measures blood flow in the fetal brain to assess for anemia.
Treatment and Management
Preventive Measures:
- Rho(D) Immune Globulin (RhoGAM): An injection given to Rh-negative women during pregnancy and after delivery of an Rh-positive baby to prevent sensitization.
- Typically administered around 28 weeks of pregnancy and within 72 hours after delivery.
- Also given after any event where fetal blood could mix with maternal blood (e.g., miscarriage, amniocentesis, abdominal trauma).
- Rho(D) Immune Globulin (RhoGAM): An injection given to Rh-negative women during pregnancy and after delivery of an Rh-positive baby to prevent sensitization.
Management of Sensitized Pregnancies:
- Frequent Monitoring: Regular ultrasounds and blood tests to monitor the health of the fetus.
- Intrauterine Transfusion: In severe cases, the fetus may receive blood transfusions while still in the womb.
- Early Delivery: If the fetus develops severe anemia or other complications, early delivery may be necessary.
Risks and Complications
For the Mother:
- Development of Rh antibodies, complicating future pregnancies.
- Risk of sensitization increases with each Rh-positive pregnancy without prophylaxis.
For the Baby:
- Anemia
- Jaundice
- Severe complications like hydrops fetalis, heart failure, and even stillbirth if untreated.
Postpartum Care
- Continued Monitoring: Babies born with HDN may need phototherapy for jaundice, blood transfusions, or other treatments.
- Future Pregnancies: Rh-negative women should receive RhoGAM in each subsequent Rh-positive pregnancy to prevent sensitization and related complications.
Conclusion
Rh-negative pregnancy requires careful management to prevent Rh incompatibility and protect the health of both the mother and the baby. With proper prenatal care, including RhoGAM injections and regular monitoring, most cases can be managed effectively, minimizing risks and complications. Women should discuss their Rh status with their healthcare provider early in pregnancy to ensure appropriate preventive measures are taken.
Copper T Insertion
Overview
Copper T insertion refers to the placement of a Copper T intrauterine device (IUD), a long-acting reversible contraceptive method. The Copper T IUD is a T-shaped plastic device wrapped with copper wire that is placed inside the uterus to prevent pregnancy.
Mechanism of Action
The Copper T IUD works primarily by releasing copper ions, which create an environment in the uterus and fallopian tubes that is toxic to sperm, inhibiting their mobility and preventing fertilization. It also induces a mild inflammatory reaction that further prevents sperm from reaching and fertilizing an egg.
Procedure
Preparation:
- Medical History and Examination: The healthcare provider will review the patient’s medical history, including any risk factors or contraindications for IUD use, and perform a pelvic examination.
- Consent: The procedure, benefits, risks, and alternatives will be explained to the patient, and informed consent will be obtained.
Insertion Process:
- Positioning: The patient will lie on an examination table with feet placed in stirrups.
- Speculum Insertion: A speculum is inserted into the vagina to allow visualization of the cervix.
- Cervical Cleaning: The cervix and vagina are cleaned with an antiseptic solution.
- Cervical Stabilization: The cervix is grasped with a tenaculum to stabilize it.
- Measurement: A uterine sound is used to measure the depth of the uterine cavity.
- IUD Insertion: The Copper T IUD is loaded into an applicator tube, which is then inserted through the cervical canal into the uterus. The IUD is released from the tube, and the applicator is withdrawn.
- Trimming the Strings: The strings attached to the IUD are trimmed so that they extend slightly into the vagina, allowing for future IUD checks and removal.
Post-Insertion:
- Observation: The patient may rest for a short period to ensure there are no immediate complications.
- Instructions: The patient is advised on what to expect, how to check for the IUD strings, and when to seek medical attention if necessary.
Benefits
- Long-Acting: Provides effective contraception for up to 10 years.
- Highly Effective: Over 99% effective at preventing pregnancy.
- Non-Hormonal: Suitable for women who cannot use hormonal contraception.
- Immediate Return to Fertility: Fertility returns quickly after removal.
- Convenient: Requires no daily or monthly action once inserted.
Risks and Side Effects
- Discomfort: Some pain or cramping during and after insertion.
- Irregular Bleeding: Spotting and irregular periods, especially in the first few months.
- Heavier Periods: Some women may experience heavier and longer menstrual periods.
- Expulsion: The IUD can be expelled from the uterus, especially in the first year.
- Perforation: Rarely, the IUD can perforate the uterine wall during insertion.
- Infection: Slightly increased risk of pelvic inflammatory disease (PID) in the first few weeks after insertion.
Contraindications
- Active Pelvic Infection: Current PID or sexually transmitted infection.
- Uterine Abnormalities: Structural abnormalities of the uterus.
- Unexplained Vaginal Bleeding: Investigate and diagnose before considering insertion.
- Copper Allergy: Known hypersensitivity to copper.
Follow-Up
- Check-Up: A follow-up visit after the first menstrual period post-insertion to ensure the IUD is in place and there are no complications.
- Regular Self-Checks: Patients should regularly check for the IUD strings in the vagina to ensure the device remains in place.
- Annual Exams: Routine annual exams to monitor the IUD and overall reproductive health.
Conclusion
Copper T insertion is a reliable and effective method of long-term contraception. It is a non-hormonal option that is suitable for many women. Proper insertion technique, patient education, and follow-up care are essential to maximize benefits and minimize risks associated with Copper T IUD use. Women considering this contraceptive method should discuss with their healthcare provider to determine if it is the right choice for their needs and circumstances.
Multiload Insertion
Overview
Multiload insertion refers to the placement of a Multiload intrauterine device (IUD), a long-acting reversible contraceptive. The Multiload IUD is a small, plastic, and copper device that is placed in the uterus to prevent pregnancy. It has a unique shape with flexible arms that help it stay in place.
Mechanism of Action
The Multiload IUD works by releasing copper ions, which create an inhospitable environment for sperm, inhibiting their motility and viability. This prevents sperm from reaching and fertilizing an egg. Additionally, the presence of the IUD induces a mild inflammatory reaction in the uterine lining that also helps prevent implantation.
Procedure
Preparation:
- Medical History and Examination: A healthcare provider will take a detailed medical history and perform a pelvic exam to ensure there are no contraindications for IUD use.
- Consent: The procedure, including benefits, risks, and alternatives, will be explained, and informed consent will be obtained.
Insertion Process:
- Positioning: The patient lies on an examination table with feet in stirrups.
- Speculum Insertion: A speculum is inserted into the vagina to visualize the cervix.
- Cervical Cleaning: The cervix and vagina are cleaned with an antiseptic solution.
- Cervical Stabilization: The cervix is grasped with a tenaculum to stabilize it.
- Measurement: A uterine sound is used to measure the depth of the uterine cavity.
- IUD Insertion: The Multiload IUD is loaded into an applicator tube, which is then gently inserted through the cervical canal into the uterus. The IUD is released from the applicator, and the tube is withdrawn.
- Trimming the Strings: The IUD strings are trimmed to an appropriate length so they extend slightly into the vagina, allowing for future checks and removal.
Post-Insertion:
- Observation: The patient may rest briefly to ensure no immediate complications.
- Instructions: The patient is advised on what to expect, how to check for the IUD strings, and when to seek medical attention if necessary.
Benefits
- Long-Acting: Provides effective contraception for 5 to 8 years, depending on the model.
- Highly Effective: Over 99% effective in preventing pregnancy.
- Non-Hormonal: Suitable for women who cannot or prefer not to use hormonal contraception.
- Immediate Return to Fertility: Fertility returns quickly after removal.
- Convenient: Requires no daily or monthly action once inserted.
Risks and Side Effects
- Discomfort: Some pain or cramping during and immediately after insertion.
- Irregular Bleeding: Spotting and irregular periods, particularly in the first few months.
- Heavier Periods: Some women may experience heavier and longer menstrual periods.
- Expulsion: The IUD can be expelled from the uterus, especially within the first year.
- Perforation: Rarely, the IUD can perforate the uterine wall during insertion.
- Infection: Slightly increased risk of pelvic inflammatory disease (PID) in the first few weeks after insertion.
Contraindications
- Active Pelvic Infection: Current PID or sexually transmitted infection.
- Uterine Abnormalities: Structural abnormalities of the uterus.
- Unexplained Vaginal Bleeding: Must be investigated and diagnosed before considering insertion.
- Copper Allergy: Known hypersensitivity to copper.
Follow-Up
- Check-Up: A follow-up visit after the first menstrual period post-insertion to ensure the IUD is in place and there are no complications.
- Regular Self-Checks: Patients should regularly check for the IUD strings in the vagina to ensure the device remains in place.
- Annual Exams: Routine annual exams to monitor the IUD and overall reproductive health.
Conclusion
Multiload insertion is a reliable and effective long-term contraceptive option. It provides a non-hormonal choice for women seeking extended protection against pregnancy. Proper insertion technique, patient education, and follow-up care are crucial to ensure the benefits of the Multiload IUD while minimizing risks. Women should consult with their healthcare provider to determine if this method is suitable for their needs and circumstances.
Medical Termination of Pregnancy (MTP)
Overview
Medical Termination of Pregnancy (MTP) refers to the use of medications to end a pregnancy. This method is typically used in the early stages of pregnancy, usually up to 10 weeks gestation. MTP is a non-invasive option compared to surgical methods and involves taking prescribed medications under medical supervision.
Indications
- Unintended Pregnancy: A common reason for seeking MTP.
- Health Risks: When continuing the pregnancy poses a risk to the mother’s health.
- Fetal Abnormalities: When the fetus has been diagnosed with abnormalities incompatible with life or causing significant morbidity.
- Psychosocial Reasons: Factors related to the woman’s mental, social, or economic conditions.
Medications Used
Mifepristone: An antiprogestin that blocks the hormone progesterone, which is necessary for pregnancy continuation. It causes the lining of the uterus to break down and the pregnancy to detach.
Misoprostol: A prostaglandin analog that induces uterine contractions to expel the pregnancy. It is taken 24-48 hours after mifepristone.
Procedure
Pre-Procedure Assessment:
- Medical History and Examination: Detailed history and physical examination to confirm pregnancy and determine eligibility for MTP.
- Ultrasound: To confirm intrauterine pregnancy and estimate gestational age.
- Laboratory Tests: Blood tests, including complete blood count and blood type, especially Rh factor status.
Administration of Medications:
- Day 1: Mifepristone (200 mg) is taken orally under medical supervision.
- Day 2-3: Misoprostol (800 mcg) is taken buccally, sublingually, or vaginally, depending on the protocol and patient preference.
Post-Medication Monitoring:
- Observation: The patient may be observed for a few hours after taking misoprostol to manage any immediate side effects.
- Symptoms to Expect: Cramping and heavy bleeding are common as the body expels the pregnancy tissue. Nausea, vomiting, diarrhea, and chills may also occur.
Follow-Up:
- Clinical Visit: A follow-up visit is typically scheduled 1-2 weeks after taking misoprostol to ensure the abortion is complete and to monitor for complications.
- Ultrasound: May be performed to confirm that the uterus is empty.
Benefits
- Non-Invasive: Avoids surgical procedures and anesthesia.
- Privacy: Can be done in the privacy of one’s home after the initial medical consultation.
- High Efficacy: Effective in approximately 95-98% of cases when used within the recommended gestational age.
Risks and Side Effects
- Incomplete Abortion: May require a follow-up surgical procedure if the abortion is incomplete.
- Heavy Bleeding: Significant bleeding may require medical attention.
- Infection: Rarely, infection can occur, requiring antibiotic treatment.
- Gastrointestinal Symptoms: Nausea, vomiting, and diarrhea are common.
- Emotional and Psychological Impact: Some women may experience emotional distress and should have access to counseling and support services.
Contraindications
- Ectopic Pregnancy: MTP is not effective for ectopic pregnancies and requires different management.
- Adrenal Failure: Mifepristone is contraindicated in patients with chronic adrenal failure.
- Allergy: Known hypersensitivity to mifepristone, misoprostol, or other prostaglandins.
- Coagulopathy: Disorders that affect blood clotting or the use of anticoagulants may increase the risk of bleeding.
Conclusion
Medical Termination of Pregnancy is a safe and effective method for ending an early pregnancy. It offers a non-invasive alternative to surgical procedures, with high efficacy and the advantage of privacy. Proper medical supervision, patient education, and follow-up care are essential to manage the procedure effectively and minimize risks. Women considering MTP should consult with their healthcare provider to ensure it is the appropriate option for their individual circumstances.
Tubal Ligation
Overview
Tubal ligation, commonly known as “getting your tubes tied,” is a surgical procedure for permanent female sterilization. It involves cutting, tying, or otherwise blocking the fallopian tubes to prevent eggs from reaching the uterus for fertilization. This method is highly effective at preventing pregnancy.
Indications
- Permanent Contraception: Chosen by women who are certain they do not want future pregnancies.
- Medical Reasons: Advised for women whose health could be severely compromised by pregnancy.
- End-of-Family Planning: Often chosen by women who have completed their families.
Procedure
Pre-Procedure Preparation:
- Medical History and Physical Examination: Comprehensive assessment to ensure the patient is a suitable candidate for the procedure.
- Informed Consent: Detailed discussion about the procedure, including its permanence, benefits, risks, and alternatives.
Surgical Methods:
- Laparoscopy: The most common method, involving small incisions and the use of a laparoscope (a thin tube with a camera).
- Steps:
- Small incisions are made in the abdomen, usually near the navel.
- The abdomen is inflated with gas to provide a better view.
- The laparoscope and surgical instruments are inserted.
- The fallopian tubes are then cut, tied, clipped, or sealed with an electric current.
- Steps:
- Mini-Laparotomy: Typically performed postpartum.
- Steps:
- A small incision is made below the navel.
- The fallopian tubes are brought through the incision, then cut and tied.
- Steps:
- Open Surgery (Laparotomy): Less common, typically used if a woman is undergoing another abdominal surgery.
- Steps:
- A larger incision is made in the abdomen.
- The fallopian tubes are cut, tied, clipped, or sealed.
- Steps:
- Laparoscopy: The most common method, involving small incisions and the use of a laparoscope (a thin tube with a camera).
Post-Procedure:
- Recovery: The patient is monitored for a few hours post-surgery. Most women can go home the same day.
- Care Instructions: Patients receive instructions on wound care, activity restrictions, and signs of complications to watch for.
- Follow-Up: A follow-up appointment may be scheduled to check healing and address any concerns.
Benefits
- Permanent Solution: Provides a permanent method of contraception.
- Highly Effective: Over 99% effective in preventing pregnancy.
- No Ongoing Maintenance: Unlike other contraceptive methods that require daily, weekly, or monthly attention.
Risks and Complications
- Surgical Risks: As with any surgery, there are risks of infection, bleeding, and adverse reactions to anesthesia.
- Postoperative Pain: Some women may experience pain or discomfort after the procedure.
- Ectopic Pregnancy: Although rare, if pregnancy does occur, it is more likely to be ectopic (in the fallopian tubes).
- Regret: Some women may regret the decision, especially if circumstances change, but reversal is often not possible or not guaranteed to restore fertility.
- Incomplete Procedure: Very rarely, the tubes may not be completely blocked, resulting in possible pregnancy.
Contraindications
- Uncertainty about Future Fertility: Women who are not absolutely certain they want permanent contraception should consider other methods.
- Medical Conditions: Conditions that increase surgical risks might contraindicate tubal ligation.
- Current Pelvic Infections: Active infections in the pelvic region should be treated before considering surgery.
Alternatives
- Reversible Contraception: Options like IUDs, contraceptive implants, birth control pills, patches, and injections.
- Vasectomy: A permanent contraception method for male partners.
Conclusion
Tubal ligation is a safe, effective, and permanent method of female sterilization. It is best suited for women who are certain they do not want future pregnancies. Proper preoperative counseling, understanding the permanence of the procedure, and awareness of potential risks and benefits are crucial. Women considering tubal ligation should have a thorough discussion with their healthcare provider to ensure it aligns with their long-term reproductive goals.