Best Laparoscopic Surgeon in Noida
Laparoscopic Ventral Hernia Repair (IPOM)
Overview
Laparoscopic ventral hernia repair, using the Intraperitoneal Onlay Mesh (IPOM) technique, is a minimally invasive procedure to repair ventral hernias. A ventral hernia occurs when there is a weakness or gap in the abdominal wall, allowing internal organs or tissues to protrude. The IPOM technique involves placing a mesh inside the abdominal cavity to cover and reinforce the hernia defect.
Indications
- Ventral Hernias: Including umbilical, incisional, and epigastric hernias.
- Recurrent Hernias: Hernias that have returned after previous repair.
- Large or Complex Hernias: Where simple suturing is not sufficient to close the defect.
Procedure Steps
Preoperative Preparation:
- Medical Evaluation: Comprehensive assessment including physical examination, imaging studies (such as CT scan or ultrasound), and preoperative lab tests.
- Informed Consent: Discussion of the procedure, potential risks, benefits, and alternatives with the patient.
Anesthesia:
- The procedure is performed under general anesthesia.

3. Surgical Technique:
- Incision and Access: Small incisions (ports) are made in the abdominal wall to insert a laparoscope (a thin, flexible camera) and surgical instruments.
- Hernia Reduction: The hernia sac and contents are reduced back into the abdominal cavity.
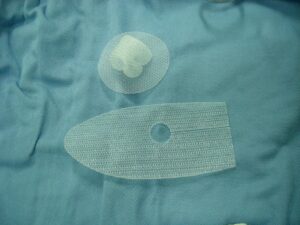
- Mesh Placement: A synthetic mesh is placed over the hernia defect from the inside of the abdominal cavity. The mesh is secured using sutures, tacks, or glue to ensure it stays in place.
- Closure: The small incisions are closed with sutures or surgical glue.
Benefits
- Minimally Invasive: Smaller incisions result in less postoperative pain, reduced risk of infection, and faster recovery compared to open surgery.
- Reduced Recurrence: The use of mesh reinforcement reduces the risk of hernia recurrence.
- Shorter Hospital Stay: Many patients can go home the same day or after a short hospital stay.
- Improved Cosmetic Outcomes: Smaller scars and less visible surgical marks.
Risks and Complications
- Infection: Though lower than with open surgery, there is still a risk of infection.
- Seroma: Accumulation of fluid at the surgical site.
- Adhesions: Formation of scar tissue that can cause bowel obstruction or chronic pain.
- Mesh Complications: Potential for mesh infection, migration, or erosion.
- Recurrence: Despite the use of mesh, there is still a small risk of hernia recurrence.
- Anesthesia Risks: As with any procedure requiring general anesthesia, there are risks related to anesthesia.
Postoperative Care
Recovery:
- Patients typically spend a few hours in the recovery room and may be discharged the same day or after an overnight stay.
- Pain management includes oral pain relievers.
Activity Restrictions:
- Patients are advised to avoid heavy lifting and strenuous activity for several weeks.
- Light activities and walking are encouraged to promote healing and prevent complications.
Follow-Up:
- Follow-up visits are scheduled to monitor healing and ensure there are no complications.
- Patients should report any signs of infection, severe pain, or other unusual symptoms to their healthcare provider promptly.
Conclusion
Laparoscopic ventral hernia repair using the IPOM technique offers a minimally invasive option for treating ventral hernias with the benefits of reduced pain, shorter recovery times, and lower risk of recurrence compared to traditional open repair. As with any surgical procedure, it is important for patients to discuss the potential benefits and risks with their healthcare provider to determine the best treatment approach for their individual needs.
Laparoscopic Cholecystectomy
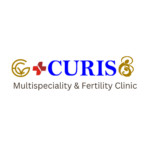
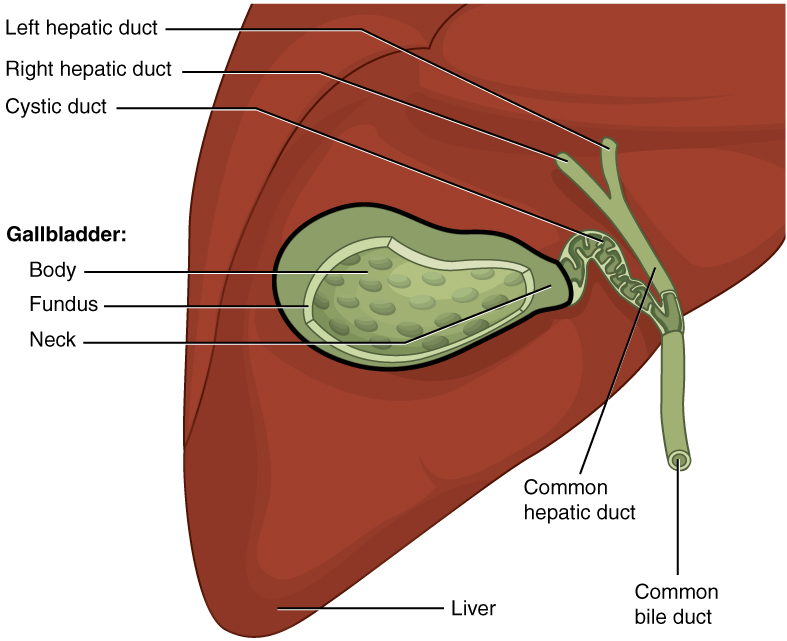
Overview
Laparoscopic cholecystectomy is a minimally invasive surgical procedure to remove the gallbladder. The gallbladder is a small, pear-shaped organ located below the liver on the upper right side of the abdomen. It stores bile, a digestive fluid produced by the liver. This procedure is commonly performed to treat gallstones and other gallbladder-related conditions.
Indications
- Gallstones: Presence of stones in the gallbladder (cholelithiasis) causing pain, infection, or inflammation.
- Cholecystitis: Inflammation of the gallbladder, often due to gallstones.
- Gallbladder Polyps: Non-cancerous growths that may become symptomatic.
- Biliary Dyskinesia: Dysfunction of the gallbladder without stones, leading to pain.
- Gallbladder Cancer: Rarely, in early-stage gallbladder cancer.
Procedure Steps
Preoperative Preparation:
- Medical Evaluation: Includes a thorough medical history, physical examination, blood tests, and imaging studies (such as ultrasound or MRI).
- Informed Consent: Discussion with the patient about the procedure, risks, benefits, and alternatives.
Anesthesia:
- The procedure is performed under general anesthesia.
Surgical Technique:
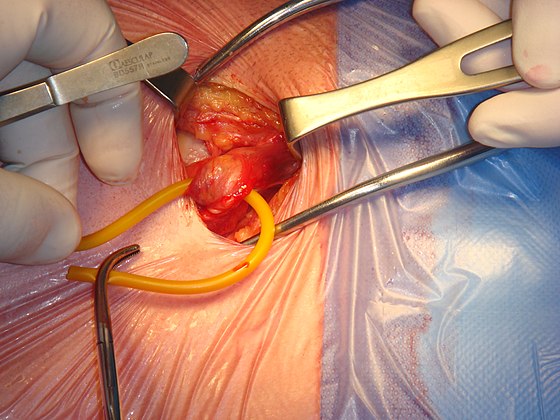
- Incision and Access: Four small incisions (ports) are made in the abdomen to insert a laparoscope (a thin, flexible camera) and specialized surgical instruments.
- Gallbladder Dissection: The surgeon visualizes the gallbladder and its surrounding structures. The cystic duct and cystic artery are identified, clipped, and cut.
- Gallbladder Removal: The gallbladder is carefully separated from the liver bed and removed through one of the small incisions.
- Closure: The small incisions are closed with sutures or surgical glue.
Benefits
- Minimally Invasive: Smaller incisions result in less postoperative pain, reduced risk of infection, and quicker recovery compared to open surgery.
- Shorter Hospital Stay: Many patients can go home the same day or after an overnight stay.
- Faster Recovery: Patients often return to normal activities within a week.
- Improved Cosmetic Outcomes: Smaller scars and less visible surgical marks.
Risks and Complications
- Infection: Though lower than with open surgery, there is still a risk of infection.
- Bile Duct Injury: Accidental injury to the bile duct can occur, leading to bile leakage or stricture.
- Bleeding: Risk of bleeding during or after surgery.
- Gallstones in Bile Duct: Residual stones may cause symptoms if left in the bile duct.
- Anesthesia Risks: As with any procedure requiring general anesthesia, there are risks related to anesthesia.
- Postcholecystectomy Syndrome: Some patients may experience digestive symptoms after gallbladder removal, such as diarrhea or bloating.
Postoperative Care
Recovery:
- Patients typically spend a few hours in the recovery room and may be discharged the same day or after an overnight stay.
- Pain management includes oral pain relievers.
Activity Restrictions:
- Patients are advised to avoid heavy lifting and strenuous activity for several weeks.
- Light activities and walking are encouraged to promote healing and prevent complications.
Diet:
- Initially, a light diet is recommended, gradually returning to normal eating habits.
- Some patients may need to avoid fatty or spicy foods if they experience digestive discomfort.
Follow-Up:
- Follow-up visits are scheduled to monitor healing and ensure there are no complications.
- Patients should report any signs of infection, severe pain, jaundice, or other unusual symptoms to their healthcare provider promptly.

Conclusion
Laparoscopic cholecystectomy is a safe and effective procedure for removing the gallbladder with the benefits of reduced pain, shorter recovery times, and improved cosmetic outcomes compared to traditional open surgery. As with any surgical procedure, it is important for patients to discuss the potential benefits and risks with their healthcare provider to determine the best treatment approach for their individual needs.
Laparoscopic Appendectomy (Appendix Surgery)
Overview
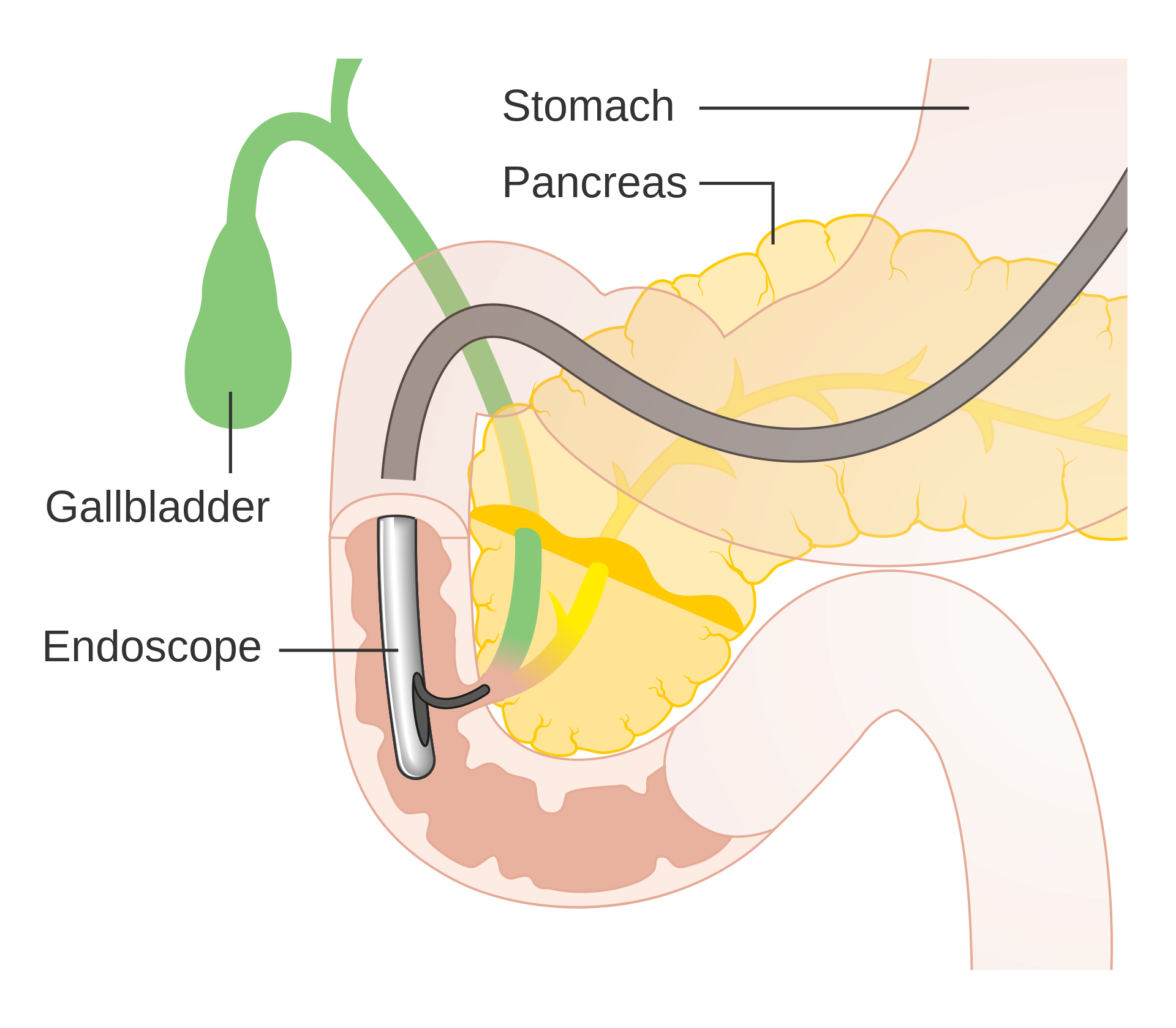
Laparoscopic appendectomy is a minimally invasive surgical procedure to remove the appendix, a small, tube-like structure attached to the large intestine. This procedure is commonly performed to treat appendicitis, which is an inflammation of the appendix that can cause severe abdominal pain and potentially lead to serious complications if not treated promptly.
Indications
- Acute Appendicitis: Inflammation of the appendix, typically presenting with pain in the lower right abdomen, fever, and nausea.
- Appendiceal Abscess: A collection of pus that forms due to a ruptured appendix.
- Appendiceal Tumors: Rarely, tumors in the appendix may necessitate removal.
Procedure Steps
Preoperative Preparation:
- Medical Evaluation: Includes a thorough medical history, physical examination, blood tests, and imaging studies (such as ultrasound or CT scan).
- Informed Consent: Discussion with the patient about the procedure, risks, benefits, and alternatives.
Anesthesia:
- The procedure is performed under general anesthesia.
Surgical Technique:
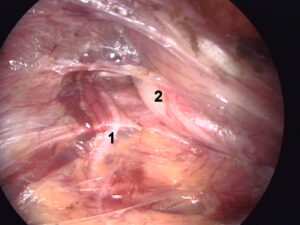
- Incision and Access: Three small incisions (ports) are made in the abdomen to insert a laparoscope (a thin, flexible camera) and specialized surgical instruments.
- Appendix Identification: The surgeon visualizes the appendix and assesses its condition.
- Appendix Removal: The blood supply to the appendix is clipped and cut. The appendix is then separated from the cecum (the beginning of the large intestine) and removed through one of the small incisions.
- Closure: The small incisions are closed with sutures or surgical glue.

Benefits
- Minimally Invasive: Smaller incisions result in less postoperative pain, reduced risk of infection, and quicker recovery compared to open surgery.
- Shorter Hospital Stay: Many patients can go home the same day or after an overnight stay.
- Faster Recovery: Patients often return to normal activities within a week.
- Improved Cosmetic Outcomes: Smaller scars and less visible surgical marks.
Risks and Complications
- Infection: Though lower than with open surgery, there is still a risk of infection.
- Bowel Injury: Accidental injury to the intestines can occur, potentially leading to complications.
- Bleeding: Risk of bleeding during or after surgery.
- Abscess Formation: Infection and pus formation in the abdominal cavity.
- Anesthesia Risks: As with any procedure requiring general anesthesia, there are risks related to anesthesia.
Postoperative Care
Recovery:
- Patients typically spend a few hours in the recovery room and may be discharged the same day or after an overnight stay.
- Pain management includes oral pain relievers.
Activity Restrictions:
- Patients are advised to avoid heavy lifting and strenuous activity for several weeks.
- Light activities and walking are encouraged to promote healing and prevent complications.
Diet:
- Initially, a light diet is recommended, gradually returning to normal eating habits.
- Patients should stay hydrated and avoid foods that can cause digestive discomfort.
Follow-Up:
- Follow-up visits are scheduled to monitor healing and ensure there are no complications.
- Patients should report any signs of infection, severe pain, or other unusual symptoms to their healthcare provider promptly.
Conclusion
Laparoscopic appendectomy is a safe and effective procedure for removing the appendix, with the benefits of reduced pain, shorter recovery times, and improved cosmetic outcomes compared to traditional open surgery. As with any surgical procedure, it is important for patients to discuss the potential benefits and risks with their healthcare provider to determine the best treatment approach for their individual needs.
Laparoscopic Inguinal Hernia Surgery (TAPP/TEP)
Overview
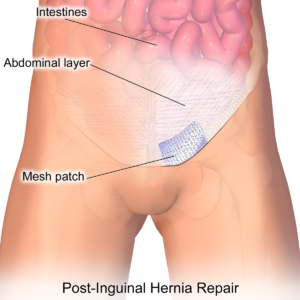
Laparoscopic inguinal hernia surgery is a minimally invasive procedure to repair inguinal hernias, which occur when a portion of the intestine or other tissue protrudes through a weak spot in the abdominal muscles near the groin. Two common laparoscopic techniques are Transabdominal Preperitoneal (TAPP) and Totally Extraperitoneal (TEP) repairs.
Indications
- Inguinal Hernias: Both direct and indirect inguinal hernias causing symptoms like pain or discomfort, bulging in the groin, or complications such as incarceration or strangulation.
- Recurrent Hernias: Hernias that have returned after previous repair.
- Bilateral Hernias: Hernias on both sides of the groin.
Procedure Steps
Preoperative Preparation:
- Medical Evaluation: Includes a thorough medical history, physical examination, blood tests, and imaging studies (such as ultrasound or CT scan).
- Informed Consent: Discussion with the patient about the procedure, risks, benefits, and alternatives.
Anesthesia:
- The procedure is performed under general anesthesia.
Surgical Technique:
- Transabdominal Preperitoneal (TAPP):
- Incision and Access: An infraumbilical incision is made, and a 10-12 mm trocar is inserted to access the peritoneal cavity. Additional small incisions are made for inserting the laparoscope and surgical instruments.
- Dissection and Mesh Placement: The peritoneum is dissected to create a preperitoneal space. The hernia sac is reduced, and a synthetic mesh is placed over the defect. The peritoneum is then closed over the mesh.
- Closure: The small incisions are closed with sutures or surgical glue.
- Transabdominal Preperitoneal (TAPP):
- Incision and Access: Small incisions are made below the umbilicus to create a working space without entering the peritoneal cavity. A balloon dissector may be used to separate the tissue layers.
- Dissection and Mesh Placement: The preperitoneal space is created, and the hernia sac is reduced. A synthetic mesh is placed over the hernia defect and secured.
- Closure: The small incisions are closed with sutures or surgical glue.

Benefits
- Minimally Invasive: Smaller incisions result in less postoperative pain, reduced risk of infection, and quicker recovery compared to open surgery.
- Lower Recurrence Rates: The use of mesh reinforcement reduces the risk of hernia recurrence.
- Shorter Hospital Stay: Many patients can go home the same day or after an overnight stay.
- Improved Cosmetic Outcomes: Smaller scars and less visible surgical marks.
- Quicker Return to Normal Activities: Patients often return to work and normal activities within a few days to a week.
Risks and Complications
- Infection: Though lower than with open surgery, there is still a risk of infection.
- Bleeding: Risk of bleeding during or after surgery.
- Chronic Pain: Persistent pain in the groin area.
- Hematoma: Collection of blood at the surgical site.
- Mesh Complications: Potential for mesh infection, migration, or erosion.
- Recurrence: Despite the use of mesh, there is still a small risk of hernia recurrence.
- Anesthesia Risks: As with any procedure requiring general anesthesia, there are risks related to anesthesia.
Postoperative Care
Recovery:
- Patients typically spend a few hours in the recovery room and may be discharged the same day or after an overnight stay.
- Pain management includes oral pain relievers.
Activity Restrictions:
- Patients are advised to avoid heavy lifting and strenuous activity for several weeks.
- Light activities and walking are encouraged to promote healing and prevent complications.
Follow-Up:
- Follow-up visits are scheduled to monitor healing and ensure there are no complications.
- Patients should report any signs of infection, severe pain, or other unusual symptoms to their healthcare provider promptly.
Conclusion
Laparoscopic inguinal hernia repair using TAPP or TEP techniques offers a minimally invasive option for treating inguinal hernias with the benefits of reduced pain, shorter recovery times, and improved cosmetic outcomes compared to traditional open repair. As with any surgical procedure, it is important for patients to discuss the potential benefits and risks with their healthcare provider to determine the best treatment approach for their individual needs.
Laparoscopic Tubectomy (Female Sterilization)
Overview
Laparoscopic tubectomy, also known as laparoscopic tubal ligation, is a minimally invasive surgical procedure for female sterilization. This procedure involves blocking, clamping, or severing the fallopian tubes to prevent eggs from traveling from the ovaries to the uterus, thereby preventing pregnancy. It is considered a permanent form of contraception.
Indications
- Permanent Contraception: Women who are certain they do not want to conceive in the future.
- Medical Conditions: Women for whom pregnancy would pose a serious health risk.
Procedure Steps
Preoperative Preparation:
- Medical Evaluation: Includes a thorough medical history, physical examination, blood tests, and possibly a pregnancy test to confirm non-pregnancy status.
- Informed Consent: Discussion with the patient about the procedure, risks, benefits, and alternatives, ensuring that the patient understands the permanence of the procedure.
Anesthesia:
- The procedure is performed under general anesthesia.
Surgical Technique:
- Incision and Access: A small incision is made near the navel to insert a laparoscope (a thin, flexible camera). Additional small incisions may be made in the lower abdomen to insert specialized surgical instruments.
- Visualization and Access to Fallopian Tubes: The laparoscope allows the surgeon to visualize the fallopian tubes. The abdominal cavity is inflated with carbon dioxide gas to provide better visibility and space to work.
- Blocking the Fallopian Tubes: The surgeon may use one of several methods to block the fallopian tubes:
- Clipping or Banding: Small clips or bands are placed around each tube to block them.
- Electrocautery: A small portion of each tube is burned to create a blockage.
- Cutting and Tying: The tubes are cut and tied to prevent the passage of eggs.
- Closure: The small incisions are closed with sutures or surgical glue.

Benefits
- Permanent Contraception: Provides a permanent solution for birth control.
- Minimally Invasive: Smaller incisions result in less postoperative pain, reduced risk of infection, and quicker recovery compared to traditional open surgery.
- Short Procedure Time: The surgery typically takes less than an hour.
- Quick Recovery: Many patients can return to normal activities within a few days.
Risks and Complications
- Infection: Though lower than with open surgery, there is still a risk of infection.
- Bleeding: Risk of bleeding during or after surgery.
- Anesthesia Risks: As with any procedure requiring general anesthesia, there are risks related to anesthesia.
- Ectopic Pregnancy: In the rare event of sterilization failure, there is a higher risk of ectopic pregnancy (pregnancy occurring outside the uterus).
- Postoperative Pain: Temporary abdominal or shoulder pain due to the gas used to inflate the abdomen.
- Regret: Some women may regret the decision, especially if they change their mind about wanting children in the future.
Postoperative Care
Recovery:
- Patients typically spend a few hours in the recovery room and can usually go home the same day.
- Pain management includes oral pain relievers.
Activity Restrictions:
- Patients are advised to avoid heavy lifting and strenuous activity for a few days.
- Light activities and walking are encouraged to promote healing and prevent complications.
Follow-Up:
- Follow-up visits are scheduled to monitor healing and ensure there are no complications.
- Patients should report any signs of infection, severe pain, or other unusual symptoms to their healthcare provider promptly.
Conclusion
Laparoscopic tubectomy is a safe and effective method for permanent female sterilization with the benefits of reduced pain, shorter recovery times, and improved cosmetic outcomes compared to traditional open surgery. It is important for patients to thoroughly discuss the potential benefits and risks with their healthcare provider and consider the permanence of the procedure before deciding on this form of contraception.
Laparoscopic Surgery at Curis Multispeciality & Fertility Clinic
Curis Multispeciality & Fertility Clinic is known as the best clinic for laparoscopic surgery in Noida. We offer advanced care in a clean, safe, and patient-friendly environment. Our team, led by the best laparoscopic surgeon in Noida, provides reliable surgical treatment with less pain and faster recovery.
Whether you need a simple procedure or a complex one, we are here to guide you at every step. We understand your concerns and focus on providing comfort and clear answers throughout your treatment.
What is Laparoscopic Surgery?
Laparoscopic surgery is also called minimally invasive surgery. It uses a small camera and tools to perform the surgery through tiny cuts. This type of surgery causes less pain, fewer scars, and helps you heal faster. At the best clinic for laparoscopic surgery in Noida, we perform various laparoscopic procedures safely and carefully.
The best laparoscopic surgeon in Noida at Curis uses the latest equipment and follows high safety standards. This helps reduce risks and gives better results for each patient.
Why Choose Curis Multispeciality & Fertility Clinic?
There are many reasons why Curis is called the best clinic for laparoscopic surgery in Noida:
- Experienced Surgeons: Our team is led by the best laparoscopic surgeon in Noida who has years of hands-on experience.
- Modern Equipment: We use high-quality machines and tools for every laparoscopic procedure.
- Quick Recovery: Because our surgeries are minimally invasive, patients recover faster and can return to normal life sooner.
- Affordable Cost: We provide world-class care without high prices.
- Clean & Safe Environment: Hygiene and patient safety are top priorities at our clinic.
People from all parts of Noida and nearby areas trust us as the best clinic for laparoscopic surgery in Noida.
Laparoscopic Procedures We Offer
At our clinic, the best laparoscopic surgeon in Noida performs many types of surgeries. Each surgery is done with care and attention.
Here are some procedures available at Curis:
- Laparoscopic Gallbladder Removal
This surgery removes the gallbladder when you have stones or other problems. It is safe, quick, and effective.
- Laparoscopic Hernia Repair
We treat different types of hernias using safe and tested methods. Our surgeon makes sure the surgery is done with less pain.
- Laparoscopic Appendectomy
This procedure removes the appendix. Our expert team at the best clinic for laparoscopic surgery in Noida ensures the process is smooth.
- Laparoscopic Hysterectomy
It is a surgery to remove the uterus. It is done for women facing long-term problems. Our clinic offers this procedure with high success rates.
- Diagnostic Laparoscopy
This is done to check what is wrong inside your abdomen. It helps to find the cause of pain, swelling, or infertility.
Each surgery is handled by the best laparoscopic surgeon in Noida who has performed hundreds of successful surgeries.
Benefits of Laparoscopic Surgery
When done at the best clinic for laparoscopic surgery in Noida, laparoscopic surgery has many benefits:
- Smaller Cuts: Very small cuts reduce pain and speed up healing.
- Less Pain: Patients feel less pain during recovery.
- Short Hospital Stay: Many patients go home the same day or next day.
- Fewer Complications: With experienced care, the risk of infection and bleeding is very low.
- Quick Return to Normal Life: You can get back to work and daily life much sooner.
Our patients always share good experiences with the best laparoscopic surgeon in Noida because of these clear advantages.
Who Needs Laparoscopic Surgery?
You may need laparoscopic surgery if:
- You have gallstones or gallbladder pain.
- You have an appendix problem.
- You have a hernia.
- You face gynecological problems like fibroids or cysts.
- You have unexplained abdominal pain.
If your doctor has advised surgery, visiting the best clinic for laparoscopic surgery in Noida will ensure safe and proper care. The best laparoscopic surgeon in Noida will examine your case and guide you through the process.
How We Ensure Patient Comfort
We take extra care of each patient. Before surgery, we explain everything clearly so you know what to expect. During surgery, the best laparoscopic surgeon in Noida uses gentle and careful techniques. After surgery, we give full support for your recovery.
Curis is known as the best clinic for laparoscopic surgery in Noida because of our kind approach and personal care. We treat every patient like family.
What to Expect Before and After Surgery
Before Surgery:
- Full check-up by the best laparoscopic surgeon in Noida.
- Detailed explanation of the surgery process.
- Basic tests to check your health.
After Surgery:
- You may rest in the clinic for a few hours or overnight.
- Our team will guide you on what to eat and how to take care.
- Most patients feel better within a few days.
- You will visit the best laparoscopic surgeon in Noida for a follow-up check.
At the best clinic for laparoscopic surgery in Noida, we make sure every step is clear and easy for you.
Our Team
The strength of Curis lies in its people. Our surgeons, nurses, and support staff work together to make sure you are well cared for. The best laparoscopic surgeon in Noida has trained under top doctors and has years of success stories behind them.
Our clinic is well-organized and patient-friendly. You will always find someone ready to help, answer your questions, and guide you.
Patient Reviews
Many patients call us the best clinic for laparoscopic surgery in Noida because of their good results. Here are a few examples:
- “I had gallbladder surgery here. The care was excellent. The best laparoscopic surgeon in Noida treated me. I recovered quickly!”
- “Curis is truly the best clinic for laparoscopic surgery in Noida. The team is caring, and everything went smoothly.”
These reviews reflect the trust and satisfaction that patients feel after treatment.
Book Your Appointment
If you or a loved one needs laparoscopic surgery, do not wait. Visit the best clinic for laparoscopic surgery in Noida and meet the best laparoscopic surgeon in Noida. We will answer all your questions and help you start your journey toward better health.
You can call us, book online, or walk into our clinic for an appointment. We are here to serve you with respect, care, and the best medical support.