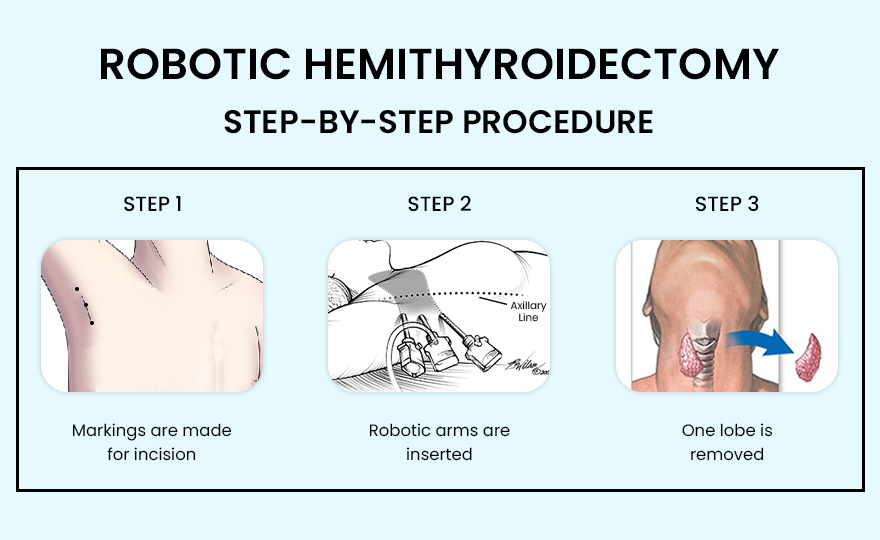
Hemithyroidectomy for Thyroid Cancer
Procedure
A hemithyroidectomy, also known as a unilateral thyroid lobectomy, involves the surgical removal of one lobe of the thyroid gland. This procedure is commonly performed under general anesthesia and includes the following steps:
Preoperative Preparation: The patient undergoes preoperative evaluations, which may include blood tests, ultrasound, fine-needle aspiration biopsy, and sometimes other imaging studies to assess the thyroid nodule or cancer.
Incision: The surgeon makes an incision in the front of the neck, typically in a natural skin crease to reduce visible scarring.
Exposure: The muscles and tissues are carefully dissected to expose the affected lobe of the thyroid gland.
Lobe Removal: The surgeon removes the affected lobe along with the isthmus (the thin band of tissue connecting the two lobes) if necessary. Care is taken to avoid damaging the recurrent laryngeal nerve and the parathyroid glands.
Closure: The incision is closed with sutures or surgical glue, and a drain may be placed to remove any excess fluid.
Benefits
Preservation of Thyroid Function: By removing only one lobe of the thyroid gland, the remaining lobe can often continue to produce enough thyroid hormones, potentially avoiding the need for lifelong hormone replacement therapy.
Effective Cancer Treatment: For patients with small, localized thyroid cancers (usually less than 1 cm and classified as low-risk), a hemithyroidectomy can be an effective treatment that removes the cancerous tissue while preserving more of the thyroid gland.
Lower Risk of Complications: Compared to a total thyroidectomy, a hemithyroidectomy has a lower risk of complications such as hypocalcemia, as the parathyroid glands on the non-affected side remain intact.
Risks
Hypothyroidism: Although less common than with a total thyroidectomy, there is still a risk that the remaining thyroid lobe will not produce sufficient hormones, necessitating thyroid hormone replacement therapy.
Voice Changes: There is a risk of damage to the recurrent laryngeal nerve, which can lead to hoarseness or voice changes.
Bleeding and Infection: As with any surgery, there are risks of bleeding and infection at the surgical site.
Recurrence: There is a possibility that cancer could recur in the remaining thyroid tissue, requiring further treatment.
Anesthetic Risks: General anesthesia carries its own set of risks, including adverse reactions to medications and complications related to breathing.
Postoperative Care
Hormone Monitoring: Thyroid hormone levels will be monitored after surgery. If the remaining thyroid lobe does not produce sufficient hormones, thyroid hormone replacement therapy may be needed.
Calcium Monitoring: Calcium levels are usually monitored, though the risk of hypocalcemia is lower than with a total thyroidectomy.
Follow-Up Visits: Regular follow-up visits with an endocrinologist or surgeon are essential to monitor thyroid function, adjust medication doses if necessary, and check for any signs of cancer recurrence.
Ultrasound and Imaging: Periodic ultrasound and other imaging studies may be performed to monitor the remaining thyroid tissue for any signs of new growth or recurrence of cancer.
Hemithyroidectomy is a valuable surgical option for treating certain cases of thyroid cancer, particularly when the cancer is localized and of low risk. This procedure aims to effectively treat the cancer while preserving as much thyroid function as possible, thereby minimizing the need for lifelong hormone replacement therapy and reducing the risk of surgical complications. Proper preoperative assessment, meticulous surgical technique, and diligent postoperative care are critical for achieving optimal outcomes.
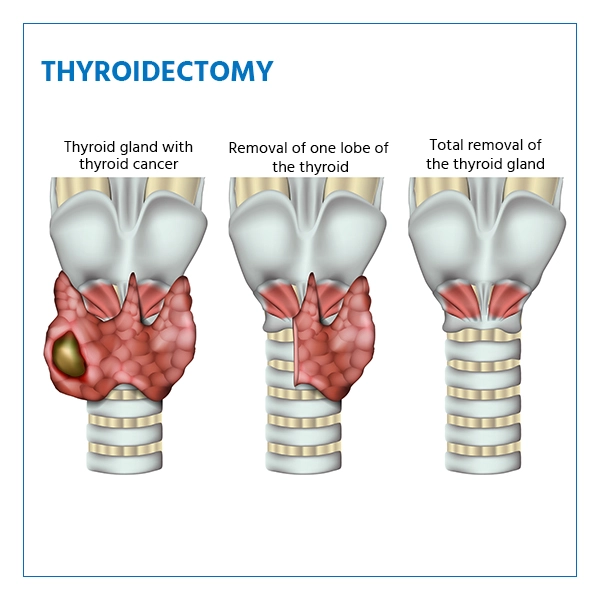
Total (MNG) and Thyroid Cancers
Procedure
A total thyroidectomy is a surgical procedure in which the entire thyroid gland is removed. This operation is performed under general anesthesia and involves the following steps:
Preoperative Preparation: The patient undergoes a series of preoperative tests, including blood tests, imaging studies (such as ultrasound or CT scans), and sometimes a fine-needle aspiration biopsy to evaluate the thyroid condition.
Incision: The surgeon makes an incision in the front of the neck, typically in a natural skin crease to minimize visible scarring.
Exposure: The muscles and tissues are carefully separated to expose the thyroid gland.
Gland Removal: The surgeon meticulously removes the thyroid gland, taking care to avoid damaging the recurrent laryngeal nerves (which control the vocal cords) and the parathyroid glands (which regulate calcium levels).
Closure: The incision is closed with sutures or surgical glue, and a drain may be placed to remove any excess fluid.
Benefits
Cancer Treatment: For patients with thyroid cancer, removing the entire gland eliminates the primary source of cancer cells, which can be essential for curing the disease or preventing its spread.
Symptom Relief: In cases of multinodular goiter, a total thyroidectomy can relieve symptoms such as difficulty swallowing, breathing issues, and cosmetic concerns related to neck swelling.
Prevention of Recurrence: By removing the entire thyroid gland, the risk of recurrence of thyroid cancer or regrowth of goiter is minimized.
Improved Diagnosis: Post-surgical histopathological examination of the entire gland can provide a definitive diagnosis and help in planning further treatment if necessary.
Risks
Hypocalcemia: Temporary or permanent hypocalcemia (low calcium levels) can occur if the parathyroid glands are damaged or inadvertently removed during surgery.
Voice Changes: Damage to the recurrent laryngeal nerves can lead to hoarseness, voice changes, or, in rare cases, loss of voice.
Bleeding and Infection: As with any surgical procedure, there is a risk of bleeding and infection at the surgical site.
Hypothyroidism: After a total thyroidectomy, patients will require lifelong thyroid hormone replacement therapy to compensate for the loss of the thyroid gland’s hormone production.
Anesthetic Risks: General anesthesia carries its own set of risks, including reactions to medications and complications related to breathing.
Postoperative Care
Hormone Replacement Therapy: Patients will need to take synthetic thyroid hormones (levothyroxine) daily to maintain normal metabolism and prevent symptoms of hypothyroidism.
Calcium Monitoring: Calcium levels will be monitored closely after surgery, and calcium or vitamin D supplements may be prescribed if necessary.
Follow-Up Visits: Regular follow-up visits with an endocrinologist or surgeon are essential to monitor hormone levels, adjust medication doses, and check for any signs of complications or recurrence of cancer.
Total thyroidectomy is a well-established and effective treatment for thyroid cancers and multinodular goiter. While it carries certain risks, the benefits often outweigh these, especially in cases where the disease poses significant health threats. Proper preoperative evaluation, skilled surgical technique, and diligent postoperative care are key to achieving the best outcomes for patients.
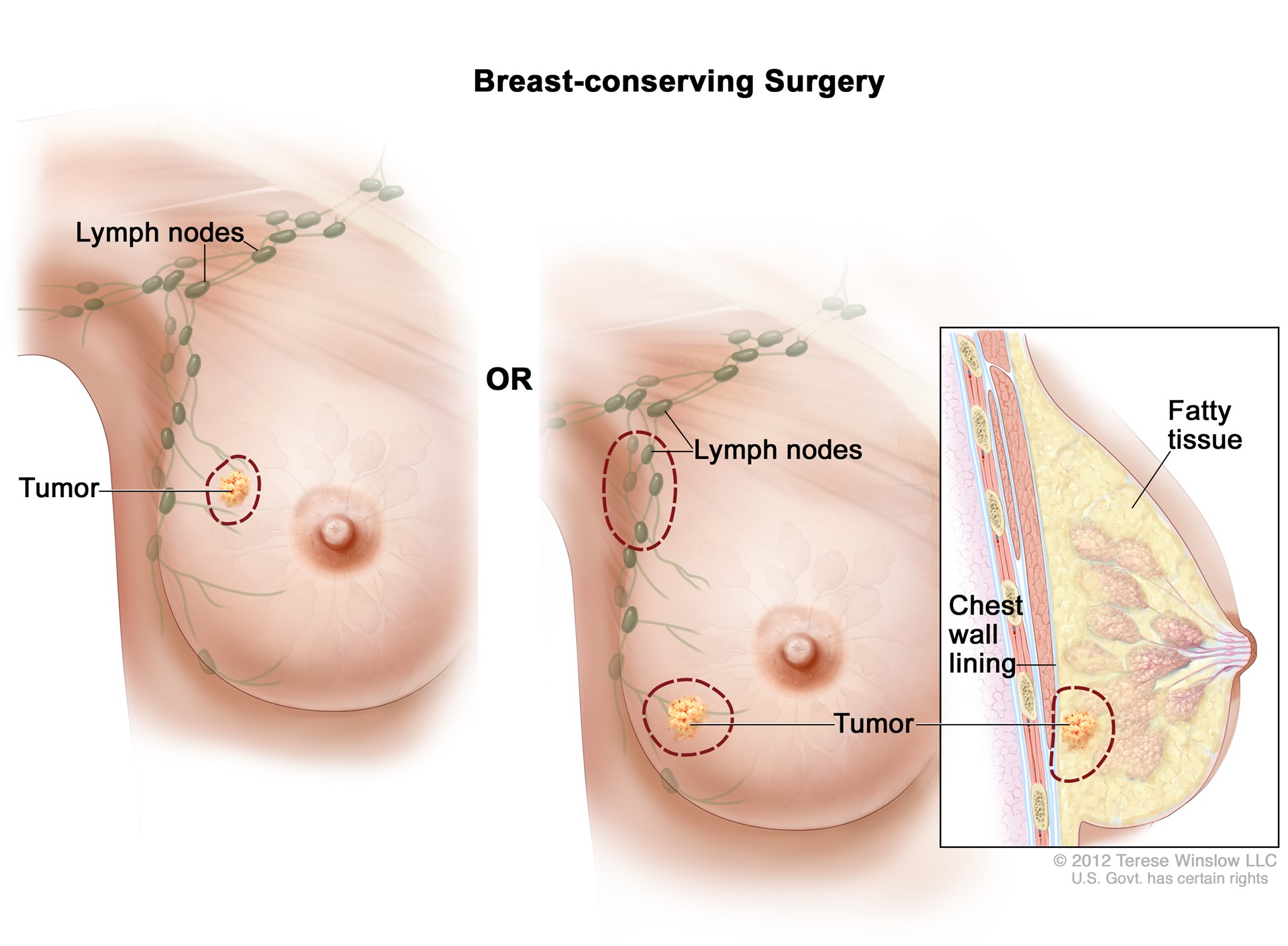
Lumpectomy (Breast Conservation Surgery)
Procedure
A lumpectomy, also known as breast-conserving surgery, is a surgical procedure designed to remove a breast tumor and a small margin of surrounding healthy tissue while preserving as much of the breast as possible. The procedure is typically performed under general anesthesia and involves the following steps:
Preoperative Preparation: The patient undergoes various diagnostic tests, such as mammography, ultrasound, MRI, and biopsy, to locate and assess the tumor. Preoperative planning may include marking the tumor location on the skin.
Incision: The surgeon makes an incision over the tumor site. The location and shape of the incision depend on the size and position of the tumor as well as cosmetic considerations.
Tumor Removal: The surgeon carefully removes the tumor along with a small margin of surrounding healthy tissue to ensure all cancerous cells are excised. The removed tissue is sent to a pathology lab to confirm clear margins (no cancer cells at the edges of the tissue).
Closure: The incision is closed with sutures or surgical glue, and a sterile dressing is applied. Drains may be placed if necessary to prevent fluid buildup.
Radiation Therapy: Typically, radiation therapy is recommended after a lumpectomy to destroy any remaining cancer cells and reduce the risk of recurrence. This therapy usually starts a few weeks after surgery.
Benefits
Breast Preservation: The primary benefit of a lumpectomy is that it allows for the removal of cancerous tissue while preserving most of the breast, which can have significant cosmetic and psychological advantages for the patient.
Effective Cancer Treatment: When combined with radiation therapy, a lumpectomy has been shown to be as effective as a mastectomy (complete breast removal) for early-stage breast cancer in terms of survival rates and recurrence prevention.
Shorter Recovery Time: Lumpectomy is less invasive than a mastectomy, typically resulting in a shorter recovery period and less postoperative pain.
Risks
Infection: As with any surgery, there is a risk of infection at the incision site.
Bleeding: There may be bleeding during or after the procedure, which is usually controlled during surgery.
Changes in Breast Appearance: The breast may change in size, shape, or appearance after surgery, especially if a large amount of tissue is removed. This can sometimes be addressed with reconstructive surgery.
Radiation Side Effects: Radiation therapy, which is usually part of the treatment plan after a lumpectomy, can cause side effects such as skin irritation, fatigue, and swelling.
Recurrence: There is a small risk of cancer recurrence in the treated breast, which is why ongoing monitoring and follow-up are crucial.
Postoperative Care
Wound Care: Patients will need to keep the surgical site clean and dry, following their surgeon’s instructions for wound care. Stitches or surgical glue will usually be checked at a follow-up appointment.
Pain Management: Pain and discomfort can be managed with prescribed or over-the-counter pain relievers. It’s important to follow the surgeon’s advice on pain management.
Activity Restrictions: Patients may be advised to avoid strenuous activities and heavy lifting for a few weeks post-surgery. Gentle exercises and stretching may be recommended to maintain mobility and prevent stiffness.
Radiation Therapy: Typically, radiation therapy begins a few weeks after surgery and continues for several weeks. Patients will need to attend regular sessions and manage any side effects with the help of their healthcare team.
Follow-Up Visits: Regular follow-up appointments are essential to monitor the healing process, assess for any signs of recurrence, and discuss ongoing breast cancer surveillance strategies.
Support Services: Psychological support and counseling services may be beneficial, as dealing with breast cancer and its treatment can be emotionally challenging. Support groups and patient education programs can also provide valuable information and support.
A lumpectomy is a key component of breast-conserving therapy, offering effective cancer treatment while allowing patients to maintain their breast appearance and quality of life. With careful surgical technique, appropriate adjuvant therapy, and diligent postoperative care, many patients can achieve excellent outcomes.
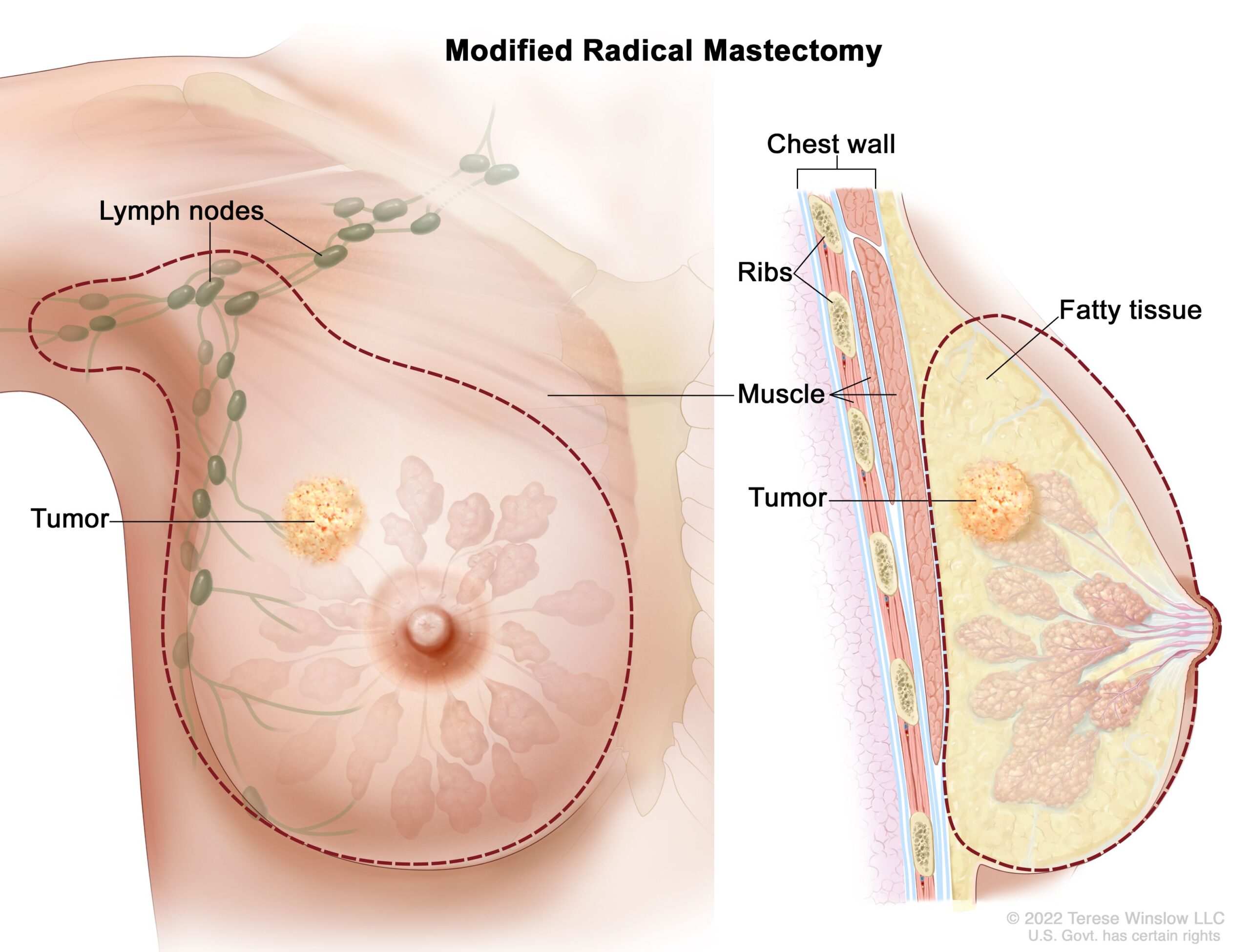
Modified Radical Mastectomy (MRM) for Breast Cancer
Procedure
A modified radical mastectomy (MRM) is a surgical procedure used to treat breast cancer by removing the entire breast, including the breast tissue, skin, areola, and nipple, as well as most of the lymph nodes under the arm (axillary lymph nodes). Unlike a radical mastectomy, the chest muscles (pectoralis major and minor) are preserved. This surgery is typically performed under general anesthesia and involves the following steps:
Preoperative Preparation: The patient undergoes various diagnostic tests, such as mammography, ultrasound, MRI, and biopsy, to evaluate the extent of the cancer. Preoperative consultations with the surgical team and anesthesiologist are conducted to plan the procedure.
Incision: The surgeon makes an incision in the breast, usually in a curved shape that follows the natural contours of the breast for better cosmetic results post-surgery.
Breast and Lymph Node Removal: The entire breast is removed, including all breast tissue, the skin, the areola, and the nipple. Additionally, most of the axillary lymph nodes are removed for examination to determine if the cancer has spread.
Closure: The incision is closed with sutures, and a sterile dressing is applied. One or more drains may be placed under the skin to remove any fluid that accumulates after surgery.
Pathological Examination: The removed breast tissue and lymph nodes are sent to a pathology lab for examination to assess the extent of the cancer and to determine if further treatment is needed.
Benefits
Comprehensive Cancer Removal: MRM effectively removes a large portion of the breast tissue and axillary lymph nodes, which can be crucial for treating and preventing the spread of breast cancer.
Assessment of Lymph Node Involvement: By removing and examining the axillary lymph nodes, doctors can better understand the extent of cancer spread and tailor subsequent treatments accordingly.
Potential for Reconstruction: Preserving the chest muscles allows for easier and more successful breast reconstruction options if the patient chooses to undergo reconstructive surgery.
Risks
Infection: As with any surgery, there is a risk of infection at the incision site.
Bleeding and Hematoma: There may be bleeding during or after the procedure, and a hematoma (a collection of blood outside the blood vessels) can form, requiring additional treatment.
Lymphedema: Removal of the axillary lymph nodes can lead to lymphedema, which is swelling in the arm due to lymph fluid buildup.
Nerve Damage: There is a risk of damage to the nerves in the chest and arm, which can cause numbness, tingling, or weakness.
Psychological Impact: The removal of a breast can have significant emotional and psychological effects, and patients may experience feelings of loss and changes in body image.
Postoperative Care
Wound Care: Patients will need to keep the surgical site clean and dry, following their surgeon’s instructions for wound care. Stitches or surgical glue will usually be checked at a follow-up appointment.
Drain Management: If drains are placed, patients will be instructed on how to care for them and measure fluid output. Drains are typically removed a few days to a week after surgery.
Pain Management: Pain and discomfort can be managed with prescribed or over-the-counter pain relievers. It’s important to follow the surgeon’s advice on pain management.
Activity Restrictions: Patients may be advised to avoid strenuous activities and heavy lifting for several weeks post-surgery. Gentle exercises and physical therapy may be recommended to maintain shoulder mobility and prevent stiffness.
Radiation Therapy and Chemotherapy: Depending on the pathology results, additional treatments such as radiation therapy, chemotherapy, hormone therapy, or targeted therapy may be recommended.
Follow-Up Visits: Regular follow-up appointments are essential to monitor healing, assess for any signs of cancer recurrence, and manage any side effects from surgery and additional treatments.
Support Services: Psychological support and counseling services are beneficial, as dealing with breast cancer and its treatment can be emotionally challenging. Support groups and patient education programs can provide valuable information and support.
Breast Reconstruction: Patients may discuss options for breast reconstruction with their surgeon. Reconstruction can be performed at the same time as the mastectomy or at a later date, depending on the patient’s preferences and medical situation.
A modified radical mastectomy is a comprehensive surgical approach for treating breast cancer, offering thorough removal of cancerous tissue while preserving important chest muscles. Proper surgical technique, postoperative care, and supportive services are essential to achieve the best possible outcomes for patients.
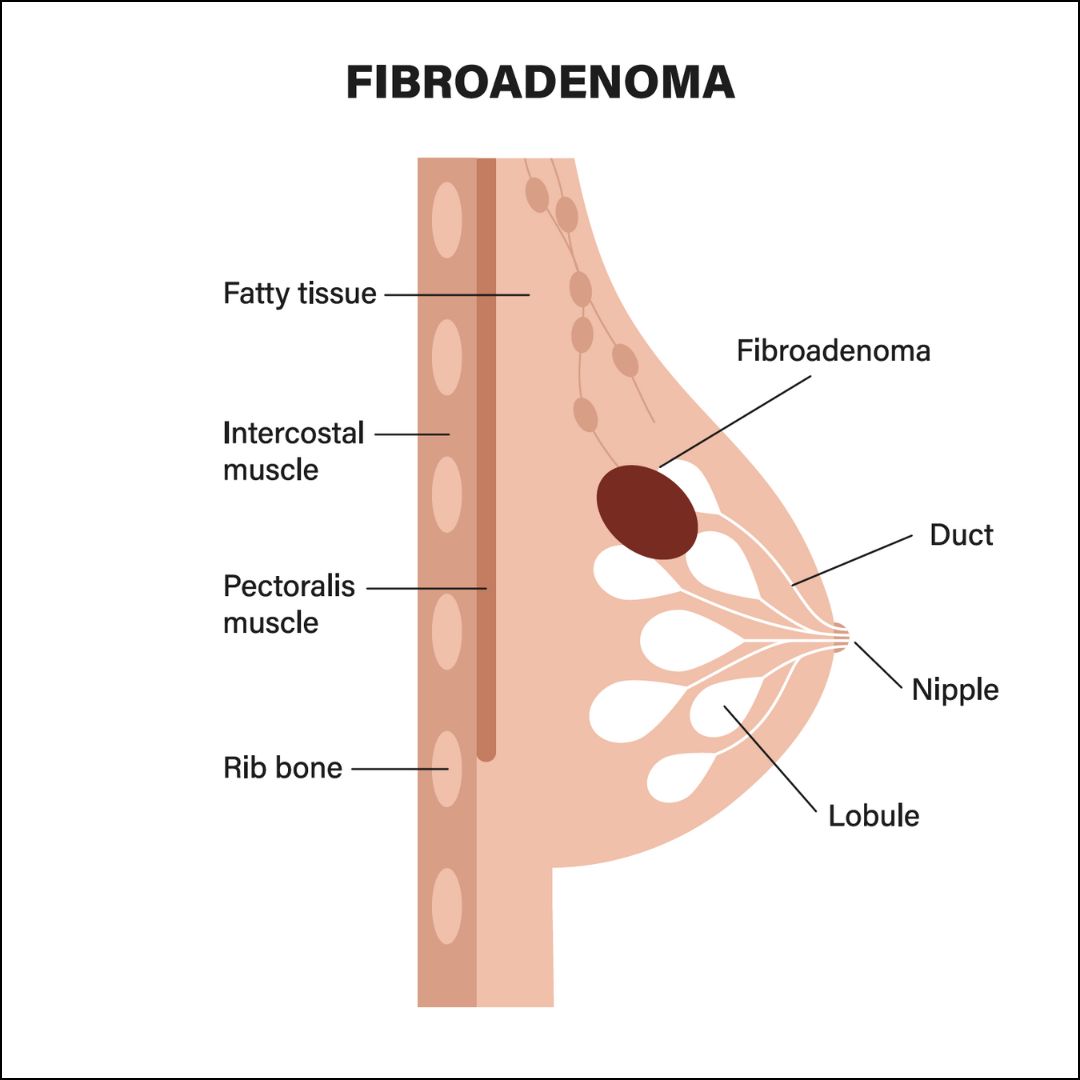
Benign Breast Lump Excision (Fibroadenomas)
Procedure
A benign breast lump excision, also known as a lumpectomy for fibroadenomas, is a surgical procedure to remove non-cancerous breast lumps. Fibroadenomas are the most common type of benign breast tumors and are typically solid, smooth, and easily movable under the skin. This procedure is usually performed under local or general anesthesia and involves the following steps:
Preoperative Preparation: The patient undergoes diagnostic tests such as mammography, ultrasound, and sometimes a core needle biopsy to confirm the lump is benign. A preoperative consultation with the surgical team is conducted to discuss the procedure.
Incision: The surgeon makes a small incision over or near the site of the fibroadenoma, typically following the natural contours of the breast to minimize visible scarring.
Lump Removal: The surgeon carefully excises the fibroadenoma along with a small margin of surrounding healthy tissue to ensure complete removal. The lump is then sent to a pathology lab for further examination.
Closure: The incision is closed with sutures, and a sterile dressing is applied. In some cases, absorbable sutures may be used, which do not require removal.
Benefits
Symptom Relief: Removing the fibroadenoma can relieve any discomfort or pain associated with the lump, especially if it is growing or causing pressure on surrounding tissues.
Peace of Mind: Excision of the lump allows for a definitive histopathological examination, providing assurance that the lump is indeed benign.
Cosmetic Outcomes: Modern surgical techniques aim to minimize scarring and preserve the natural appearance of the breast, leading to better cosmetic outcomes.
Risks
Infection: As with any surgery, there is a risk of infection at the incision site, which can usually be managed with antibiotics.
Bleeding and Hematoma: There may be bleeding during or after the procedure, and a hematoma (a collection of blood outside the blood vessels) can form, requiring additional treatment.
Scarring: There will be a scar at the site of the incision, though surgeons aim to minimize its size and visibility.
Changes in Breast Shape: Depending on the size of the fibroadenoma and the amount of tissue removed, there may be changes in the shape or contour of the breast.
Postoperative Care
Wound Care: Patients will need to keep the surgical site clean and dry, following their surgeon’s instructions for wound care. Stitches will typically be checked and possibly removed at a follow-up appointment if non-absorbable sutures are used.
Pain Management: Pain and discomfort can be managed with prescribed or over-the-counter pain relievers. Ice packs may also help reduce swelling and pain.
Activity Restrictions: Patients may be advised to avoid strenuous activities and heavy lifting for a few weeks post-surgery to allow proper healing.
Follow-Up Visits: Regular follow-up appointments are essential to monitor the healing process and check for any signs of infection or complications.
Monitoring for Recurrence: While fibroadenomas are benign, patients should continue regular breast self-examinations and screening mammograms as recommended by their healthcare provider to monitor for any new lumps or changes.
A benign breast lump excision for fibroadenomas is a relatively straightforward and effective procedure to remove non-cancerous breast lumps, providing symptom relief and peace of mind while aiming for minimal cosmetic impact. With proper surgical technique and diligent postoperative care, most patients can expect a smooth recovery and excellent outcomes.
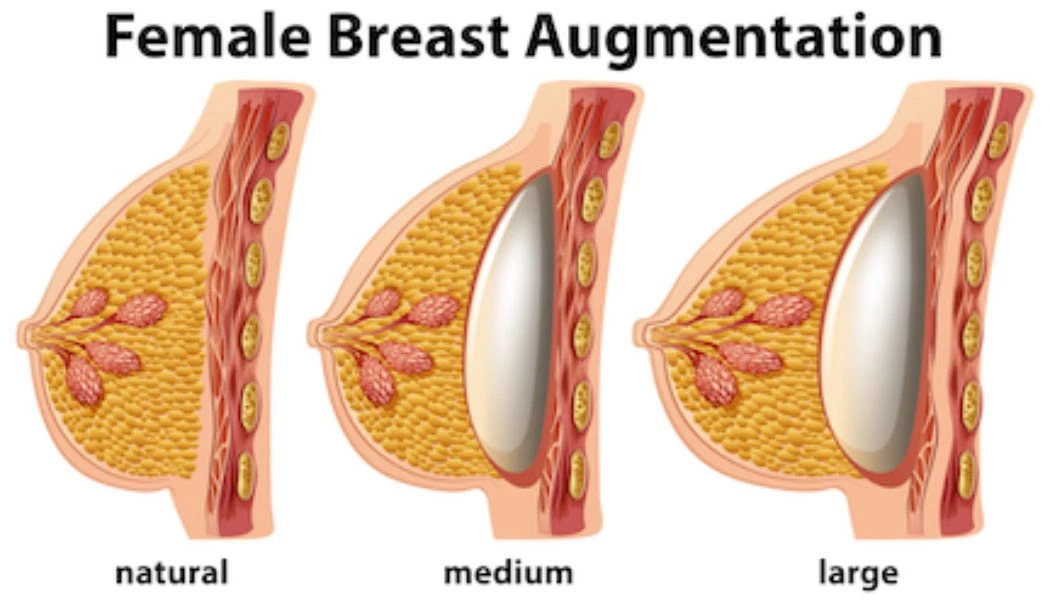
Breast Augmentation Surgery
Procedure
Breast augmentation surgery, also known as augmentation mammoplasty, is a cosmetic surgical procedure designed to enhance the size and shape of a woman’s breasts using implants or fat transfer. The procedure is typically performed under general anesthesia and involves the following steps:
Preoperative Consultation: The patient meets with the surgeon to discuss goals, implant options (saline vs. silicone), size, shape, incision sites, and placement (above or below the chest muscle). Preoperative imaging and measurements are taken.
Incision Options: The surgeon makes an incision in one of several possible locations:
- Inframammary: Under the breast along the inframammary fold.
- Periareolar: Around the lower edge of the areola.
- Transaxillary: In the armpit.
- Transumbilical (less common): Through the belly button.
Implant Placement: The breast implant is inserted into a pocket either:
- Submuscular: Under the pectoral muscle.
- Subglandular/Submammary: Over the pectoral muscle and directly behind the breast tissue.
Implant Insertion: The chosen implants (saline or silicone) are inserted through the incision and positioned properly.
Closure: The incisions are closed with sutures, skin adhesive, or surgical tape. The surgeon places dressings over the incisions and may use drainage tubes to prevent fluid buildup.
Postoperative Monitoring: The patient is monitored in a recovery area before being discharged home with specific postoperative care instructions.
Benefits
Enhanced Appearance: Breast augmentation can improve the size, shape, and symmetry of the breasts, enhancing overall body proportions and aesthetic appeal.
Boost in Self-Confidence: Many patients experience increased self-esteem and confidence following the procedure due to improved body image.
Restoration: It can restore breast volume lost due to weight reduction, pregnancy, or aging.
Reconstruction: It can be used for breast reconstruction after mastectomy or injury.
Risks
Surgical Complications: Risks include infection, bleeding, and adverse reactions to anesthesia.
Capsular Contracture: The formation of scar tissue around the implant can cause the breast to feel firm and may require corrective surgery.
Implant Rupture or Leakage: Both saline and silicone implants can rupture, necessitating replacement.
Changes in Sensation: There may be changes in breast or nipple sensation, which can be temporary or permanent.
Implant Displacement: The implants may shift from their original position, leading to asymmetry and potentially requiring revision surgery.
Unsatisfactory Results: Some patients may be dissatisfied with the aesthetic outcome and may require additional surgery.
Postoperative Care
Wound Care: Patients must keep the surgical site clean and dry, follow the surgeon’s instructions for wound care, and avoid submerging the incisions in water until they are fully healed.
Pain Management: Pain and discomfort are managed with prescribed or over-the-counter pain relievers. Swelling and bruising are common and typically subside over time.
Activity Restrictions: Patients should avoid strenuous activities and heavy lifting for several weeks post-surgery. Gentle movements and light activities are encouraged to prevent stiffness.
Wearing Support Garments: Patients are often advised to wear a support bra or compression garment to minimize swelling and support the breasts during healing.
Follow-Up Visits: Regular follow-up appointments with the surgeon are essential to monitor healing, check for complications, and assess the results.
Long-Term Care: Patients should monitor their breasts for any changes and have regular check-ups. MRI scans may be recommended every few years to check for silent ruptures in silicone implants.
Breast augmentation surgery is a popular and effective procedure for enhancing the appearance of the breasts. With proper surgical technique, thorough preoperative planning, and diligent postoperative care, patients can achieve their desired aesthetic goals and enjoy improved confidence and satisfaction with their body image.
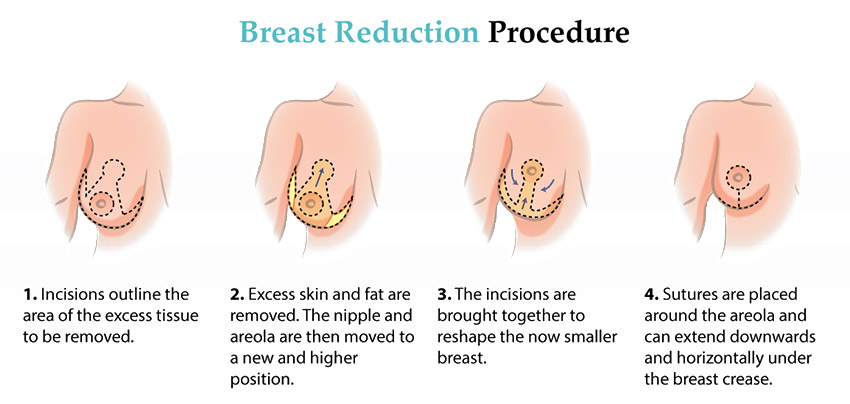
Breast Reduction Surgery
Procedure
Breast reduction surgery, also known as reduction mammoplasty, is a surgical procedure designed to reduce the size and weight of large, heavy breasts, alleviating discomfort and improving breast appearance. This procedure involves the removal of excess breast tissue, fat, and skin. It is typically performed under general anesthesia and includes the following steps:
Preoperative Consultation: The patient meets with the surgeon to discuss goals, evaluate breast size and shape, and review medical history. The surgeon will examine the breasts, take measurements, and possibly take photographs for medical records.
Marking the Incision Sites: On the day of surgery, the surgeon marks the breasts to indicate where incisions will be made and how the tissue will be removed and reshaped.
Incision Options: The surgeon makes incisions in one of several patterns, depending on the amount of reduction needed and the patient’s anatomy:
- Anchor or Inverted-T: Incisions are made around the areola, vertically down to the breast crease, and horizontally along the crease.
- Lollipop or Vertical: Incisions are made around the areola and vertically down to the breast crease.
- Donut or Periareolar: Incisions are made only around the areola.
Tissue Removal and Reshaping: The surgeon removes excess breast tissue, fat, and skin. The remaining breast tissue is reshaped to create a natural-looking, smaller breast. The nipple and areola are repositioned to a higher, more youthful location.
Closure: The incisions are closed with sutures, and the surgeon places dressings over the surgical site. Drainage tubes may be inserted to remove excess fluid.
Postoperative Monitoring: The patient is monitored in a recovery area before being discharged home with specific postoperative care instructions.
Benefits
Alleviates Physical Discomfort: Breast reduction can relieve chronic pain in the neck, back, and shoulders, as well as skin irritation under the breasts caused by large, heavy breasts.
Improved Mobility: Reducing breast size can make physical activities and exercise more comfortable and enjoyable.
Enhanced Appearance: The surgery can improve the proportion and shape of the breasts, leading to better body contour and increased confidence.
Psychological Benefits: Many patients experience a boost in self-esteem and mental well-being after the procedure due to improved physical comfort and body image.
Risks
Surgical Complications: Risks include infection, bleeding, and adverse reactions to anesthesia.
Scarring: There will be permanent scars, though they typically fade over time and are often placed in less visible areas. The extent and visibility of scars depend on the incision technique used.
Changes in Sensation: There may be changes in breast or nipple sensation, which can be temporary or permanent.
Asymmetry: There is a possibility of unevenly sized or shaped breasts, which may require additional surgery.
Difficulty Breastfeeding: Some patients may experience difficulties with breastfeeding after the surgery, depending on how much tissue is removed and the surgical technique used.
Wound Healing Issues: Delayed wound healing or wound breakdown can occur, particularly in patients who smoke or have other health issues.
Postoperative Care
Wound Care: Patients must keep the surgical site clean and dry, following their surgeon’s instructions for wound care. Stitches are typically checked and possibly removed at a follow-up appointment if non-absorbable sutures are used.
Pain Management: Pain and discomfort are managed with prescribed or over-the-counter pain relievers. Swelling and bruising are common and typically subside over time.
Activity Restrictions: Patients should avoid strenuous activities and heavy lifting for several weeks post-surgery to allow proper healing. Gentle movements and light activities are encouraged to prevent stiffness.
Wearing Support Garments: Patients are often advised to wear a support bra or compression garment to minimize swelling and support the breasts during healing.
Follow-Up Visits: Regular follow-up appointments with the surgeon are essential to monitor healing, check for complications, and assess the results.
Long-Term Care: Patients should monitor their breasts for any changes and maintain a healthy lifestyle to support overall well-being.
Breast reduction surgery is an effective solution for individuals experiencing discomfort and self-consciousness due to overly large breasts. With proper surgical technique, thorough preoperative planning, and diligent postoperative care, patients can achieve significant relief from physical symptoms and enjoy improved aesthetics and quality of life.
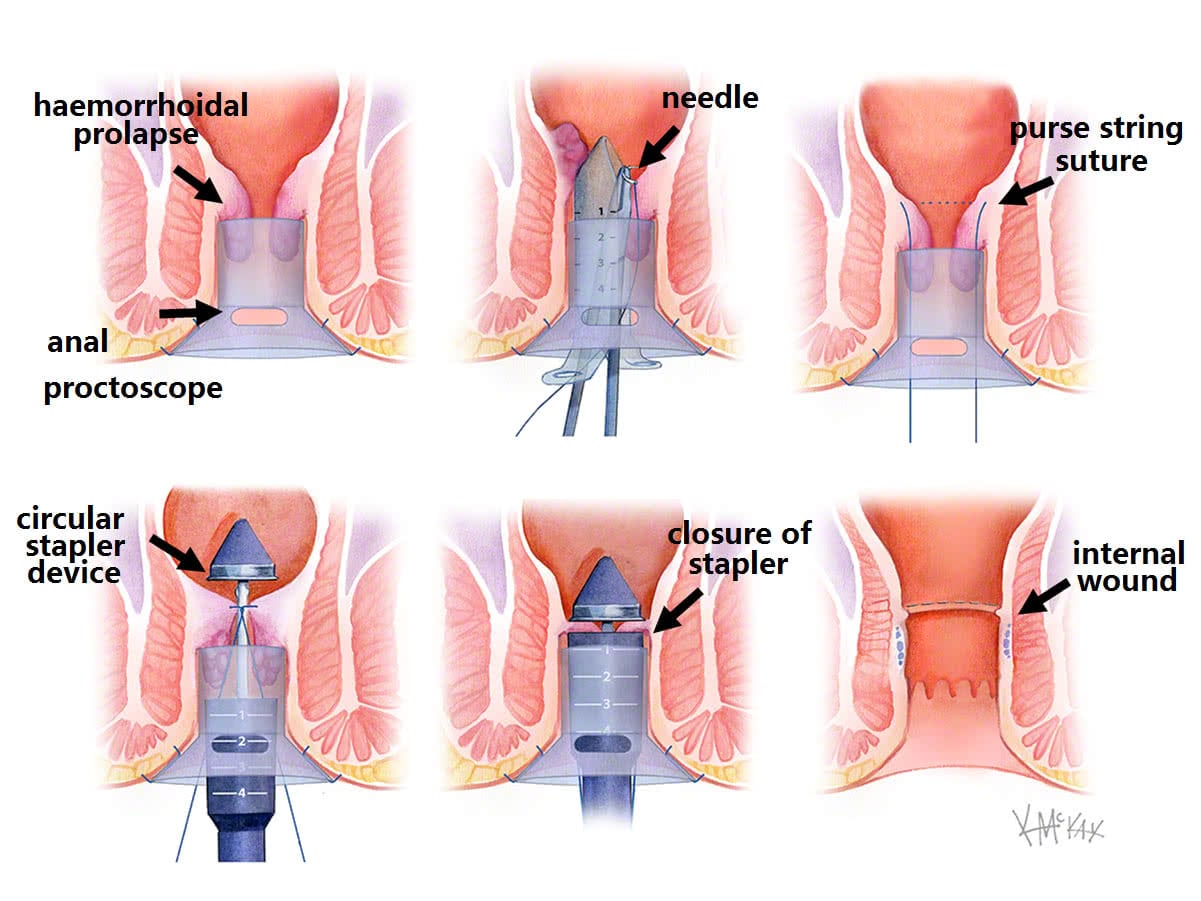
Stapled Hemorrhoidopexy (Hemorrhoids/Piles Surgery)
Procedure
Stapled hemorrhoidopexy, also known as Procedure for Prolapse and Hemorrhoids (PPH), is a minimally invasive surgical technique used to treat internal hemorrhoids by lifting and securing prolapsed hemorrhoidal tissue back into its normal position within the anal canal. This procedure is typically performed under general or regional anesthesia and involves the following steps:
Preoperative Preparation: The patient undergoes a thorough medical evaluation, including a review of medical history and a physical examination. Preoperative instructions, such as fasting and bowel preparation, are given.
Positioning and Anesthesia: The patient is positioned in the lithotomy or prone jackknife position. Anesthesia is administered to ensure the patient is comfortable and pain-free during the procedure.
Insertion of Circular Stapler: The surgeon inserts a specialized circular stapling device into the anal canal. This device is designed to remove a ring of excess hemorrhoidal tissue and reposition the remaining tissue.
Tissue Excision and Stapling: The stapler device excises a circumferential ring of prolapsed hemorrhoidal tissue and simultaneously staples the remaining tissue to lift and secure it back into its normal position. This action reduces blood flow to the hemorrhoids, causing them to shrink.
Closure: The stapling device is removed, and the surgical site is inspected for proper hemostasis (control of bleeding). Additional sutures may be placed if necessary.
Postoperative Monitoring: The patient is monitored in a recovery area before being discharged home with specific postoperative care instructions.
Benefits
Reduced Pain: Compared to traditional hemorrhoidectomy, stapled hemorrhoidopexy is associated with less postoperative pain due to the absence of large external wounds.
Faster Recovery: Patients typically experience a quicker recovery and can return to normal activities sooner than those undergoing conventional hemorrhoid surgery.
Effective Symptom Relief: The procedure effectively reduces hemorrhoidal prolapse and alleviates symptoms such as bleeding, pain, and itching.
Lower Recurrence Rate: Stapled hemorrhoidopexy has a lower recurrence rate for prolapsed hemorrhoids compared to some other treatments.
Risks
Bleeding: There is a risk of bleeding during or after the procedure, which may require additional interventions.
Infection: As with any surgical procedure, there is a risk of infection, which can be managed with antibiotics.
Anal Stricture: Narrowing of the anal canal (stricture) can occur, leading to difficulty with bowel movements.
Recurrence: While the recurrence rate is generally lower, there is still a possibility of hemorrhoids returning.
Fecal Incontinence: Rarely, patients may experience issues with bowel control following the procedure.
Pain: Although less common than with traditional hemorrhoidectomy, some patients may still experience pain after the procedure.
Postoperative Care
Pain Management: Pain and discomfort can be managed with prescribed or over-the-counter pain relievers. Patients should avoid straining during bowel movements to minimize pain.
Dietary Adjustments: A high-fiber diet and increased fluid intake are recommended to soften stools and prevent constipation. Fiber supplements may also be suggested.
Activity Restrictions: Patients should avoid strenuous activities and heavy lifting for several weeks post-surgery to allow proper healing.
Wound Care: Keeping the anal area clean and dry is crucial. Patients should follow their surgeon’s instructions for perianal hygiene.
Follow-Up Visits: Regular follow-up appointments with the surgeon are essential to monitor healing, check for complications, and assess the results.
Laxatives and Stool Softeners: These may be prescribed to help ensure smooth bowel movements and reduce strain on the surgical site.
Stapled hemorrhoidopexy is an effective and less painful alternative to traditional hemorrhoid surgery for treating internal hemorrhoids. With proper surgical technique, thorough preoperative planning, and diligent postoperative care, patients can achieve significant relief from hemorrhoidal symptoms and enjoy a quicker recovery.
Excision Surgery for Fissure, Fistula, and Pilonidal Disease
Overview
Excision surgery is a common approach for treating anal fissures, fistulas, and pilonidal disease. These conditions, while distinct, all involve the removal of problematic tissue to alleviate symptoms and prevent recurrence.
1. Anal Fissure Excision
Anal fissures are small tears in the lining of the anus that can cause pain and bleeding during bowel movements.
Procedure
Preoperative Preparation: The patient undergoes a medical evaluation, including history, physical examination, and sometimes anoscopy to confirm the diagnosis.
Anesthesia: Local, regional, or general anesthesia is administered to ensure the patient is comfortable during the procedure.
Incision and Excision: The surgeon makes a small incision to access the fissure. Depending on the chronicity and location, the surgeon may perform a lateral internal sphincterotomy, which involves cutting a small portion of the internal anal sphincter muscle to reduce spasm and promote healing.
Closure: The incision is typically left open to heal naturally, though sometimes it may be sutured.
Benefits
- Pain Relief: Immediate relief from pain associated with chronic anal fissures.
- Improved Healing: Reduces muscle spasm, allowing the fissure to heal.
Risks
- Infection: Risk of postoperative infection.
- Incontinence: Small risk of minor incontinence due to sphincterotomy.
Postoperative Care
- Pain Management: Pain relief with medications.
- Dietary Changes: High-fiber diet and increased fluid intake to prevent constipation.
- Hygiene: Keeping the area clean and dry.
2. Anal Fistula Excision
Anal fistulas are abnormal connections between the anal canal and the skin near the anus, often resulting from abscesses.
Procedure
Preoperative Preparation: Includes medical history, physical examination, and imaging studies like fistulography or MRI to map the fistula tract.
Anesthesia: Local, regional, or general anesthesia is used.
Incision and Excision: The fistula tract is identified, and an incision is made to excise the entire tract. Various techniques may be used, such as fistulotomy (opening the fistula tract) or fistulectomy (complete removal).
Closure: The wound is either left open to heal by secondary intention or closed with sutures.
Benefits
- Elimination of Infection: Removes the source of chronic infection and discharge.
- Symptom Relief: Alleviates pain and discomfort.
Risks
- Infection: Postoperative infection risk.
- Recurrence: Possibility of fistula recurrence.
- Incontinence: Potential risk depending on the fistula’s location and extent.
Postoperative Care
- Wound Care: Keeping the surgical site clean.
- Pain Management: Medications to manage pain.
- Follow-Up: Regular check-ups to monitor healing and detect recurrence.
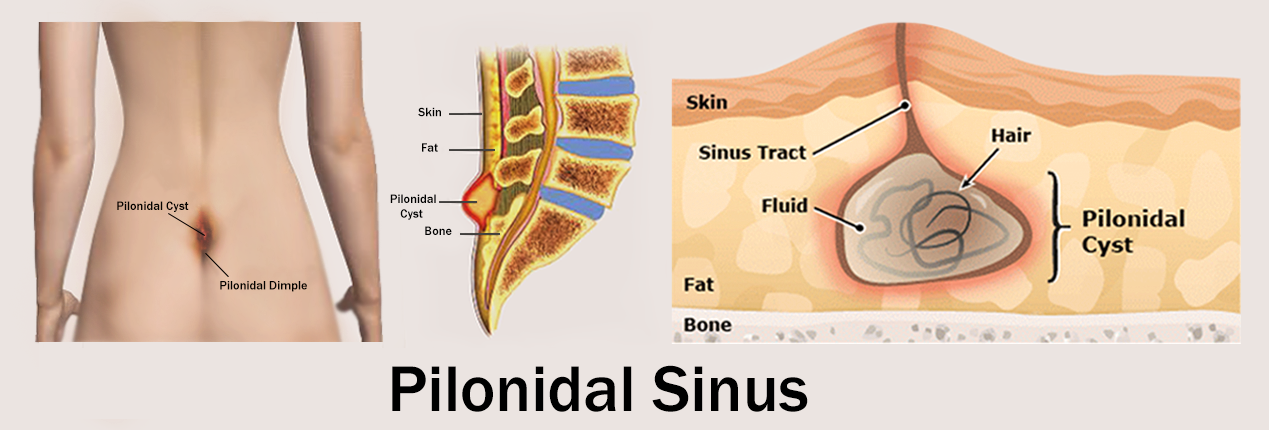
3. Pilonidal Cyst Excision
Pilonidal cysts are cysts that occur near the tailbone at the top of the buttocks cleft, often containing hair and skin debris.
Procedure
Preoperative Preparation: Medical evaluation, including history and physical examination, to confirm the diagnosis.
Anesthesia: Local, regional, or general anesthesia is administered.
Incision and Excision: The surgeon makes an incision over the cyst and removes the cyst along with the surrounding inflamed tissue.
Closure: The wound can be left open to heal by secondary intention (with packing) or closed with sutures. Sometimes, a drainage tube may be placed.
Benefits
- Symptom Relief: Alleviates pain, swelling, and infection.
- Prevents Recurrence: Complete removal reduces the risk of future cyst formation.
Risks
- Infection: Risk of postoperative infection.
- Recurrence: Pilonidal cysts can recur, especially if not all affected tissue is removed.
Postoperative Care
- Wound Care: Daily dressing changes and keeping the area clean.
- Pain Management: Pain relief with medications.
- Activity Restrictions: Avoiding prolonged sitting and activities that stress the area.
General Postoperative Care for All Procedures
- Pain Management: Use of prescribed pain relievers to manage discomfort.
- Hygiene: Maintaining cleanliness of the surgical site to prevent infection.
- Dietary Adjustments: High-fiber diet and adequate hydration to ease bowel movements (especially for anal procedures).
- Follow-Up Visits: Regular check-ups to monitor healing and detect any complications early.
- Activity Restrictions: Avoiding strenuous activities until fully healed.
Excision surgery for anal fissures, fistulas, and pilonidal disease is effective in relieving symptoms and preventing recurrence. With proper surgical technique and diligent postoperative care, patients can expect significant improvements in their condition and quality of life.
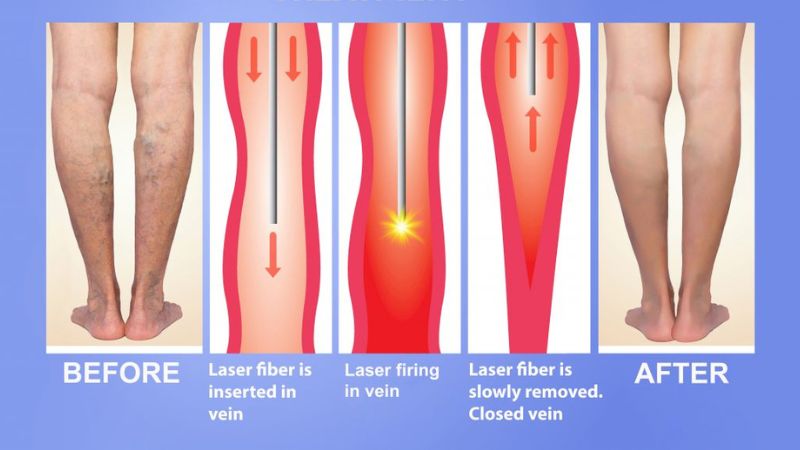
Varicose Veins Treatment with Laser or Radiofrequency Ablation (RFA)
Varicose veins are enlarged, swollen, and twisted veins that usually appear blue or dark purple on the legs and can cause discomfort or pain. Laser or radiofrequency ablation (RFA) is a minimally invasive procedure used to treat varicose veins by closing them off, redirecting blood flow to healthier veins.
Procedure
Preoperative Evaluation: The patient undergoes a medical evaluation, including history, physical examination, and possibly imaging studies such as ultrasound to assess the extent and severity of the varicose veins.
Anesthesia: Local anesthesia or tumescent anesthesia (a solution injected into the treatment area) is administered to numb the area and minimize discomfort during the procedure.
Vein Access: The surgeon makes a small incision or puncture near the affected vein and inserts a catheter or fiber-optic device into the vein under ultrasound guidance.
Ablation: With laser ablation, a laser fiber is inserted into the vein through the catheter, and laser energy is delivered to heat and close off the vein. In RFA, a radiofrequency catheter is used to deliver radiofrequency energy to heat and seal the vein.
Closure: After the ablation is complete, the catheter is slowly withdrawn, and pressure is applied to the incision site to prevent bleeding. No stitches are usually required.
Compression: Compression stockings or bandages are applied to the treated leg to help reduce swelling, promote healing, and prevent blood clots.
Benefits
- Minimally Invasive: Laser or RFA procedures are minimally invasive, requiring only a small incision or puncture.
- High Success Rate: Both laser and RFA treatments have high success rates in closing off varicose veins and relieving symptoms.
- Quick Recovery: Patients typically experience minimal discomfort and can resume normal activities within a few days to a week after the procedure.
- Cosmetic Improvement: Closure of varicose veins leads to cosmetic improvement in the appearance of the legs.
Risks
- Bruising and Discomfort: Some bruising and discomfort may occur at the treatment site, but these are usually temporary.
- Infection: Risk of infection at the incision site, though this is rare with proper postoperative care.
- Nerve Injury: There is a small risk of nerve injury during the procedure, leading to numbness or tingling in the leg, but this is rare.
- Deep Vein Thrombosis (DVT): In rare cases, DVT can occur, especially if compression stockings are not worn as recommended postoperatively.
Postoperative Care
- Compression: Wearing compression stockings as directed by the surgeon to promote healing and prevent blood clots.
- Activity: Walking and light activities are encouraged immediately after the procedure to improve circulation and prevent blood clots.
- Pain Management: Over-the-counter pain relievers can help manage any discomfort.
- Follow-Up: Regular follow-up appointments with the surgeon to monitor healing and assess the effectiveness of the treatment.
Conclusion
Laser or radiofrequency ablation is an effective and minimally invasive treatment option for varicose veins, offering high success rates, quick recovery, and cosmetic improvement. With proper preoperative evaluation, skilled surgical technique, and diligent postoperative care, patients can expect significant relief from varicose vein symptoms and improved leg appearance.
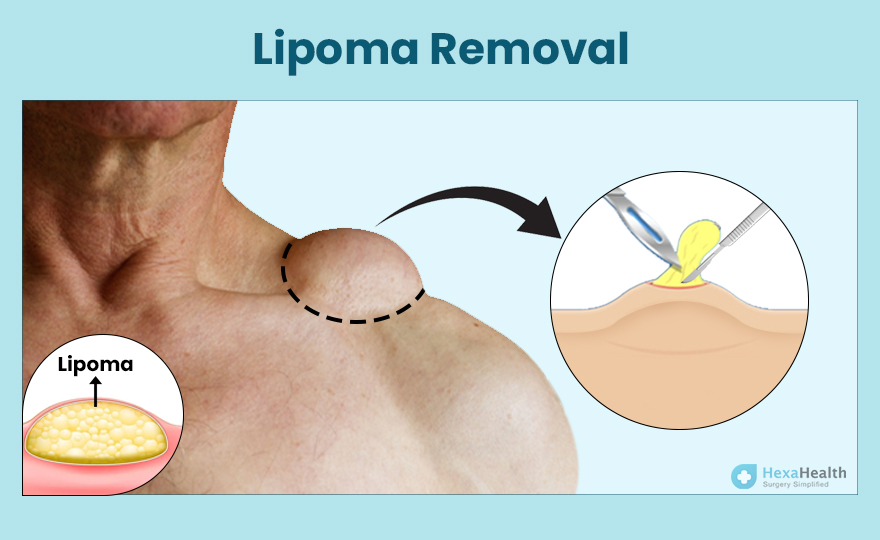
Excision Surgery for Lipomas and Cysts
Excision surgery is a common procedure used to remove lipomas and cysts, which are benign growths often found beneath the skin. Lipomas are soft, fatty lumps, while cysts are sacs filled with fluid or semi-solid material.
Procedure
Preoperative Evaluation: The patient undergoes a medical evaluation, including history and physical examination, to confirm the diagnosis and assess the size and location of the growth.
Anesthesia: Local anesthesia is typically used to numb the area where the growth is located. In some cases, depending on the size and location of the growth or patient preference, general anesthesia may be used.
Incision: The surgeon makes a small incision over the lipoma or cyst, exposing the growth and surrounding tissue.
Excision: Using surgical instruments, the surgeon carefully removes the lipoma or cyst along with any surrounding tissue if necessary to ensure complete removal. In some cases, the cyst or lipoma may be easily removed intact, while in others, it may need to be dissected out in pieces.
Closure: Once the growth is removed, the incision is closed with sutures or stitches. In some cases, the wound may be left open to heal from the inside out (secondary intention), particularly for larger cysts or infected areas.
Dressing: A sterile dressing is applied to the incision site to protect it and promote healing. If the wound is left open, it may require packing with gauze to absorb drainage.
Benefits
- Removal of Growth: Excision surgery effectively removes lipomas and cysts, eliminating any associated discomfort or cosmetic concerns.
- Prevention of Recurrence: Complete removal of the growth reduces the risk of recurrence, especially for cysts.
Risks
- Bleeding: Risk of bleeding during or after the procedure, though this is typically minimal and can be controlled by the surgeon.
- Infection: Risk of infection at the incision site, particularly if proper wound care instructions are not followed.
- Scarring: All surgical incisions will leave a scar, though the extent and visibility of the scar can vary depending on factors such as the size and location of the incision and individual healing characteristics.
- Nerve Damage: There is a small risk of nerve damage during the procedure, leading to numbness or altered sensation in the area.
Postoperative Care
- Wound Care: Keeping the surgical site clean and dry to prevent infection. The patient may need to change dressings and apply antibiotic ointment as directed by the surgeon.
- Pain Management: Over-the-counter pain relievers can help manage any discomfort. Prescription pain medication may be necessary for more significant procedures or if the patient experiences significant pain.
- Activity Restrictions: Patients may need to avoid strenuous activities or heavy lifting for a period following surgery to allow for proper healing.
- Follow-Up: Regular follow-up appointments with the surgeon to monitor healing, remove stitches if necessary, and assess the effectiveness of the procedure.
Excision surgery for lipomas and cysts is generally safe and effective, offering relief from discomfort and cosmetic concerns associated with these benign growths. With proper surgical technique and diligent postoperative care, patients can expect successful outcomes and minimal risk of complications.